A Comprehensive Analysis of Medication Errors with Antimicrobials in a Tertiary Care Hospital of Northern India
JASPI June 2024/ Volume 2/Issue 2
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
April-June 30, 2024
Sharma R, Juneja S, Saini D, Singh K. A Comprehensive Analysis of Medication Errors with Antimicrobials in a Tertiary Care Hospital of Northern India. JASPI. 2024;2(2):9-13 DOI: 10.62541/jaspi032
ABSTRACT
Background: Medication errors, resulting from incomplete understanding, pose significant risks to patient safety. Antimicrobial medication error is a global concern further exacerbated by underreporting. This study aims to determine the prevalence of antimicrobial medication errors at a tertiary care medical facility.
Methodology: A retrospective study was conducted over six months. Antimicrobial medication errors were analyzed and categorized as prescription, transcription, indenting, dispensing, and administration errors. A total of 208 antimicrobial medication errors were analyzed using the National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) risk index.
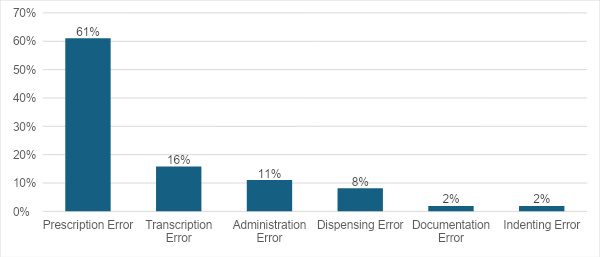
Results: Among 6,439 medication charts assessed, 558 (9%) medication errors were identified, with antimicrobial errors accounting for 208 (37.2%). Prescription errors were the most prevalent (61%), followed by transcription errors (16%) and administration errors (11%). Dispensing, indenting, and documentation errors occurred at rates of 8%, 2%, and 2%, respectively. The primary causes of errors were incorrect doses (47.2%) and frequencies (30%). Approximately 55.3% of antimicrobial medication errors were classified as Category C according to the NCCMERP risk assessment.
Conclusion: Prescription errors represent the majority of antimicrobial medication errors, underscoring the need for enhanced vigilance among consultant physicians during prescription writing and drug schedule checks.
KEYWORDS: Medication Errors; Antimicrobials Errors; Prescription Errors; Transcription Errors.
INTRODUCTION
A medication error (ME), according to the National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP), is a preventable incident that could result in wrong medication usage or harm to the patient while under the care of healthcare providers.1 These incidents encompass various aspects of healthcare, such as prescribing, labelling, dispensing, administration, monitoring, education, practices, products, and systems.2 Numerous categories exist for classifying medication errors. In healthcare settings, the most prevalent categorization approach is based on the point in the medication use process where errors occur, such as during prescription, transcription, dispensing, administration, or monitoring.3 ME can occur at any stage, from the prescription to the administration of the drug.
In India, 5.2 million injuries are attributed annually as a result of medication errors as well as adverse events. In contrast, in the US, seven thousand to ten thousand fatalities in hospitals are reported annually as a result of medication errors.4,5 The patient’s trust in the healthcare system is lowered as a result of the ME, which also raises morbidity, mortality, and costs. Various contributing factors include but not limited to it are insufficient patient data, unavailability of drug information, selecting an inappropriate drug from a list of choices, poor environment (light, temperature), misunderstandings of drug orders due to poor handwriting, conflict between medications with identical names, improper use of zeroes and decimal points, misunderstandings of metric as well as other dosing units, inappropriate abbreviations and others.6,7 The majority of ME is not harmful to the patient. Still, a small number can have unintended consequences such as short or long-term damage to the individual’s health and well-being, more extended hospital stays, higher treatment costs, loss of confidence in the healthcare delivery system, and sometimes casualties.8
The current study aimed to determine the prevalence of antimicrobial ME among patients admitted to a tertiary care facility. Since antimicrobial agents (AMAs) are the most frequently prescribed group of drugs in the current times, the current study’s objective was to assess ME prevalence as well as to identify the most typical error in general wards and surgical intensive care units (ICUs) in a tertiary care medical facility. The exclusive monitoring of AMAs is crucial, and keeping in mind, this study was planned to precisely analyze and focus on AMAs associated with ME with an intent to promote the rational use of antimicrobials.
METHODOLOGY
A retrospective study using inpatient medical records was conducted over six months, from January 1, 2023, to June 30, 2023. Data from all inpatients in general wards and surgical ICUs were included. Patients attending outpatient departments and inpatients not receiving medications were excluded. Institute Ethics Committee approval was waived due to the data collected during routine hospital audits.
Data was collected through a standard Prescription Appropriateness Review (PAR). The gathered data was analyzed to identify medication errors (ME), specifically focusing on errors associated with antimicrobial medications. The ME detected were grouped into various categories: prescription errors, transcription errors, indenting errors, dispensing errors, and administration errors (Prescription errors occur during the prescribing process, transcription errors happen when entering medication details into records, indenting errors arise during medication ordering, dispensing errors occur in pharmacy preparation, and administration errors happen when administering medication to the patients). These categories were further broken down based on their underlying causes. These causes encompassed incomplete prescriptions, illegible prescriptions, incorrect drugs, wrong dosages, improper dosing frequencies, inaccurate routes, wrong timings, inappropriate formulations, incorrect dilutions, omissions, usage of error-prone abbreviations, and therapeutic duplication. The NCCMERP risk index was used to evaluate the outcome of the ME. Category A and Category B are potential errors that cause no harm to the patient, while Category C and Category I are actual errors that harm the patient. The data entry and analysis were conducted using Microsoft Excel and the statistical program SPSS version 26. Descriptive statistics were employed to analyze the data.
RESULTS
A total of 6,439 medication charts underwent assessment, and 558 ME were identified, representing 8.66%. Of these errors, 208(37%) were associated with AMAs. Among 37% of errors, the majority were identified from general and surgical intensive care units (ICU) 56.3%, as shown in Table 1. On analysis using NCCMERP criteria, it was found that 56% of errors belonged to category C, as shown in Table 2.
Table 1: Demographic profile of patients
|
Total Antimicrobial Medication Error N=208 |
Frequency (Percent) |
|
Gender |
|
|
Male |
137(65.9) |
|
Female |
71(34.1) |
|
Age groups |
|
|
< 17 years |
10(4.8) |
|
18-64 years |
96(46.2) |
|
65-above |
102(49) |
|
Location |
|
|
ER |
12(5.8) |
|
ICU |
117(56.3) |
|
IP Pharmacy |
12(5.8) |
|
OT |
9(4.3) |
|
WARDS |
58(27.9) |
ER- Emergency, OT- operation theatre, ICU-Intensive care unit, IP Pharmacy-In Patient pharmacy
Table 2: Incident categories as per NCCMERP
|
Incident category |
Frequency (Percent) |
|
Category A |
18(8.7) |
|
Category B |
75(36.1) |
|
Category C |
115(55.3) |
|
Category D-I |
0(0) |
NCCMERP- National Coordinating Council for Medication Error Reporting and Prevention
In this study, prescription errors accounted for 127(61%) of the errors, transcription errors followed by administration errors at 33(16%) and 23(11%), respectively, as shown in Figure 1. Prescription errors accounted for 61%, which included inappropriate doses (67%), followed by therapeutic duplication (8%) and wrong frequency (6%). Transcription errors accounted for 16%, which included wrong dose (30%), wrong generic name (18%), and wrong frequency (12%), followed by missed transcription (18%). Administration errors comprised 11%, which were subcategorized as wrong frequency (34.7%), followed by missed dose (30%), and wrong dose (17.4%). Within the spectrum of antimicrobial errors, antibiotics made up the majority at 92.7%, followed by antifungal medications at 7.2%, and the remaining 1.92% accounted for other categories of AMAs, which include rifaximin, nitrofurantoin, etc. On further detailed analysis of the classification of AMAs associated with ME, it was observed that the β lactam plus carbapenem (46%) group of AMAs was associated with the highest number of errors, followed by glycopeptides (18.3%).
Figure 1: Category-wise medication errors
One probable reason may be because they are a widely used class of AMAs. The nitroimidazole class comprised 5.3% of errors, while the polyene and sulfonamide classes had the lowest error rates at 0.5% each, as shown in Table 3.
Table 3: Error rates in different antimicrobial classes
|
Antimicrobial class Frequency (percent) |
Antimicrobial class Frequency (percent) |
|
β-lactam plus carbapenem |
95(45.7) |
|
Glycopeptide |
38(18.3) |
|
Polypeptide |
16(7.7) |
|
Quinolones |
11(5.3) |
|
Nitroimidazole |
11(5.3) |
|
Macrolide |
10(4.8) |
|
Azoles |
5(2.4) |
|
Tetracyclines |
4(1.9) |
|
Other |
4(1.9) |
|
Echinocandins |
3(1.4) |
|
Oxazolidinone |
3(1.4) |
|
Aminoglycosides |
3(1.4) |
|
Antimetabolite |
2(1.0) |
|
Polyene |
1(0.5) |
|
Sulfonamide |
1(0.5) |
|
Lincosamide |
1(0.5) |
|
Total |
208 |
DISCUSSION
Medications are widely used to attain certain benefits, treat ailments, and improve an individual’s overall quality of life. ME may occur at any stage of the medication usage process, initiating from prescription and dispensing to drug administration to the patient. These errors not only elevate the morbidity and mortality rates within the population but also lead to heightened treatment costs. Additionally, they can erode a patient’s trust in the quality of medical care.9,10
According to this study, a total of 37% of AMAs associated with ME were identified. Very few studies in a similar context are available in the current literature, suggesting sparse information on AMAs associated with ME. A study in a tertiary care hospital observed 39% ME without any deaths. Similar research conducted in the Indian states of Uttarakhand and Karnataka has revealed that the ME rate in hospital patients might reach up to 25.7% and 15.34%, respectively.11,12 Sneaking at the gender distribution, males comprised 137 (66%), whereas females recognized 71 (34%) in this study. Similarly, in another study, the majority of the population were males (54%) in whom ME were reported.12
The NCCMERP harm index has been used to assess the error analysis. In the current analysis, most errors fell in category C (55%) and B (36%), similar to another study conducted in West Ethiopia, which depicted 63% category C and 20 % category B errors, respectively.13,14 Contrary to this, category B medication errors predominated, followed by category C errors in a Saudi Arabian study.15 Another study by Parthasarathi et al. reported the majority of ME falling under category A.16,17 It was found in this study that patients of age more than 60 years were more likely to experience medication errors. The probable reason for the same could be polypharmacy in the elderly population, which needs acquisitive care in terms of doses and drug interactions. A similar study by Pote et al. found that the ME were more common in people over 60 years of age.18 In contrast to the above studies, Sandeep et al. and Karna et al. found that people between the ages of 41 and 60 were prone to experience errors associated with medications.12,19
Prescription errors associated with AMAs were the most frequent errors found in this study. Illegibility was the most common reason for inappropriate doses, consistent with another study by Murthy V. et al. in Tamil Nadu.20 On the other hand, Zirpe et al. reported transcription errors as the most frequent ones, followed by prescription errors.21 In this study, administration errors accounted for 11% of AMAs associated with ME, but in a study by Sandeep. et al., the frequency of medication administration errors was 25%. Sarah et al. also revealed that the administration errors were 28%.22
This study mainly focused on AMAs associated with MEs, and the administration of other drugs was not a part of the analysis. The exclusiveness of this study comparison is difficult as more studies are explicitly required for the AMA group of drugs. This is because antimicrobials are rampantly prescribed nowadays, contributing to irrationality and leading to antimicrobial resistance, a global threat.
CONCLUSION
It is essential to identify AMAs associated with ME falling into different subcategories to promote judicious use and avoid adverse effects of this group of medications. Antimicrobial stewardship encourages responsible usage of antimicrobials, and identifying ME in AMAs can help recognize the shortfalls of antimicrobial prescriptions. This can be a future step to combat the rapidly increasing AMRs.
ACKNOWLEDGEMENT
We thank Fortis Hospital, Mohali, for providing us with the best environment and facilities to carry out this work.
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
AUTHOR’S CONTRIBUTION
RS: Conceptualization; Data collection; Literature review; Methodology; Analysis; Writing the draft; Approve
SJ: Writing the draft; Review & Editing; Approve
DS: Writing the draft; Review & Editing; Approve
KS: Validation; Review & Editing; Approve
REFERENCES
1. Devine EB, Wilson-Norton JL, Lawless NM, et al. Preparing for Ambulatory Computerized Prescriber Order Entry by Evaluating Preimplementation Medication Errors. In: Henriksen K, Battles JB, Marks ES, et al., eds. Advances in Patient Safety: From Research to Implementation. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005.
2. Tariq RA, Vashisht R, Sinha A, Scherbak Y. Medication Dispensing Errors and Prevention. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.
3. Ferner RE, Aronson JK. Clarification of terminology in medication errors: definitions and classification. Drug Saf. 2006;29(11):1011-22.
4. Wittich CM, Burkle CM, Lanier WL. Medication errors: an overview for clinicians. Mayo Clin Proc. 2014;89(8):1116-25.
5. Aashita SA, Khan ZH, Khokhar A. Basic concept of patient safety in healthcare delivery. Int J Curr Res. 2018;10(8):72926-32.
6. Sinha G, Acharya LD, Thunga G, Mathews T. A study of medication errors in general medicine wards of the South Indian tertiary care hospital. Asian Journal of Pharmaceutical and Clinical Research. 2016;9(4):196-200.
7. Donaldson MS. An Overview of To Err is Human: Re-emphasizing the Message of Patient Safety. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008.
8. Gorgich EA, Barfroshan S, Ghoreishi G, Yaghoobi M. Investigating the Causes of Medication Errors and Strategies to Prevention of Them from Nurses and Nursing Student Viewpoint. Glob J Health Sci. 2016;8(8):54448.
9. Cohen MR. Medication errors: causes, prevention, and risk management. Jones & Bartlett Learning; 2000.
10. Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533-43.
11. Gaur S, Sinha A, Srivastava B. Medication errors in medicine wards in a tertiary care teaching hospital of a hill state in India. Asian J Pharm Life Sci. 2012;2:56-63.
12. Patanwala AE, Warholak TL, Sanders AB, Erstad BL. A prospective observational study of medication errors in a tertiary care emergency department. Ann Emerg Med. 2010;55(6):522-6.
13. Patel S, Patel A, Patel V, Solanki N. Study of medication error in hospitalized patients in tertiary care hospital. Indian Journal of Pharmacy Practice. 2018;11(1):32-6.
14. Dedefo MG, Mitike AH, Angamo MT. Incidence and determinants of medication errors and adverse drug events among hospitalized children in West Ethiopia. BMC Pediatr. 2016;16:81.
15. Khoja T, Neyaz Y, Qureshi NA, Magzoub MA, Haycox A, Walley T. Medication errors in primary care in Riyadh City, Saudi Arabia. East Mediterr Health J. 2011;17(2):156-9.
16. Aldayyen AM, Alwabari MA, Alhaddad F, et al. Types, trends, and patterns of the reported antimicrobial errors to the eastern region’s medical centers in Saudi Arabia: A cross-sectional study. Saudi Pharm J. 2023;31(4):569-77.
17. Parthasarathi A, Puvvada R, Patel H, Bhandari P, Nagpal S. Evaluation of Medication Errors in a Tertiary Care Hospital of a Low- to Middle-Income Country. Cureus. 2021;13(7):e16769.
18. Pote S, Tiwari P, D’cruz S. Medication prescribing errors in a public teaching hospital in India: A prospective study. Pharm Pract (Granada). 2007;5(1):17-20.
19. Karna K, Sharma S, Inamdar SH. The impact of educational intervention strategies in reducing medication errors in a tertiary care teaching hospital–a second intervention study. Int Res J Pharma. 2012; 1-17
20. Murthy VN. Evaluation and categorization of medical errors occured in cardiology department of tertiary care hospital. J Basic Clin Pharm. 2017;8:60-3.
21. Zirpe KG, Seta B, Gholap S, et al. Incidence of Medication Error in Critical Care Unit of a Tertiary Care Hospital: Where Do We Stand? Indian J Crit Care Med. 2020;24(9):799-803.
22. Berdot S, Sabatier B, Gillaizeau F, Caruba T, Prognon P, Durieux P. Evaluation of drug administration errors in a teaching hospital. BMC Health Serv Res. 2012;12:60.
Submit a Manuscript:
Copyright © Author(s) 2024. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

