WHONET use in Indian Set Up
JASPI September 2024/ Volume 2/Issue 3
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Dash D, Rai S, Patro P.WHONET use in Indian Set Up. JASPI. 2024;2(3):1-5 DOI: 10.62541/jaspi047
KEYWORDS: Whonet; AMR; AMSP: Indian set up.
INTRODUCTION
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi, and parasites no longer respond to antimicrobial agents. As a result of drug resistance, antibiotics, and other antimicrobial drugs become ineffective, and infections become difficult or impossible to treat.
AMR is a natural process that happens over time through genetic changes in pathogens. Human activity accelerates its emergence and spread, mainly due to the misuse and overuse of antimicrobials to treat, prevent, or control infections in humans, animals, and plants.1 It has become a growing global public health challenge, with approximately 4.95 million deaths in 2019 and an estimated 10 million deaths per year by 2050 in the absence of a well-planned, coordinated approach to contain this menace.2 To have a solution to this impending catastrophe, we need to measure the problem adequately. AMR surveillance is such a measurement tool as it defines the problem of drug resistance and identifies interventions to enhance the appropriate use of antimicrobials.3 The AMR is usually detected by measuring bacterial growth in the presence of the antibiotic being tested, and subsequently, all these individual data are combined to form an antibiogram. The antibiogram is defined as the report generated by analysis of collective AST results, usually from a single healthcare facility.4 Local antibiograms, in general, and hospital antibiograms, in particular, are prerequisites for formulating the antibiotic policy of that particular hospital. WHONET can immensely help each set generate its own antibiogram in this regard.
WHONET (www.whonet.org) system is a Windows-based open-access software that curates information on antimicrobial surveillance results. It is developed and supported by the WHO Collaborating Centre for Surveillance of Antimicrobial Resistance at the Brigham and Women’s Hospital in Boston, Massachusetts, and is available in 44 languages, supports local, national, regional, and global surveillance efforts in over 2,300 hospitals, public health, animal health, and food laboratories in over 130 countries worldwide.5
WHONET SOFTWARE
The software can be installed easily on a personal computer (Windows). If any laboratory already has a computerized reporting system, data can be converted by BacLink software, which is also available free of charge from the WHO. The data structure is compatible with major databases, spreadsheets, and statistical software programs.5
The software has three main parts. First is a laboratory configuration file, which can be customized to the laboratory, an interface for data entry and a part for analyzing and reporting resistance data.6
Laboratory configuration file
This program permits the user to enter and modify laboratory-specific information such as patient care areas (outpatient department, inpatient ward, or intensive care unit), antibiotic panel selection, and interpretive breakpoints for various antibiotics according to standard guidelines. In addition, one can indicate what data fields one wants included in the data files. This configuration can be modified subsequently (Figure 1A).
Data entry
Data entry files can be configured separately based on specimen type, month-wise, year-wise, etc.
It supports routine entry of susceptibility test results performed by disk diffusion, MIC, and E-test. It has inbuilt Interpretation guidelines for most standardized testing methodologies. It also has pre-defined “Alert rules” to alert microbiologists and infection control staff of unlikely, unusual, and important findings and ensure quality and gross mistakes in result entry (Figure 1B). Currently, the WHONET has 354 pre-defined “Alert rules.”
Data analysis
An excellent feature of WHONET is its ability to analyze stored data. It can generate epidemiological data and antibiograms and also has infection control applications. The user can select the type of analysis to run, the bacteria to analyze, the subsets of isolates to include or exclude (e.g., all isolates from urine only and from specific locations), and the antimicrobial agents and period to examine (Figure 1C).
Type of analysis usually includes a percentage of data categorized as resistant, intermediate, or susceptible; distributions of test measurements (zone diameter, minimal inhibitory concentration) in the form of histograms, scatterplots, and regression curves besides comparing measurements for different agents or methods for the same isolates. Line listings of isolates grouped by combinations of agents to which they are resistant (antibiotypes) to trace distinctive strains, along with an automated screening of data for unusual isolates, can be done.6
(Figure 1A) (Figure 1B)
(Figure 1C)
WHY IS WHONET REQUIRED IN THE INDIAN SET-UP?
The usual flow of a culture & susceptibility investigation follows a sequence of identifying the organism conventionally or with the help of automated equipment in a clinical microbiology laboratory; performing antimicrobial susceptibility by disk diffusion method or minimum inhibitory concentration method(s); the measurements, their interpretive categories, and the species or subspecies identification of the tested microbe sent in as paper or electronic reports to each patient’s record to guide that patient’s therapy.7 In many resource-constrained facilities, the results are stored in paper logbooks and consequently are unavailable for supporting data analysis and data sharing. However, of late, in many low-resource settings, reports are stored in the electronic files of a laboratory information system (LIS) integrated with other clinical reporting services.7 In India, each clinical microbiology laboratory, in medical colleges, corporate set-ups or stand-alone laboratories, has years of registers/logbooks of all these organisms and their resistance pattern. When we think of national data, these are mainly unused or unshared representations of past and ongoing resistance progression. The Indian Council of Medical Research (ICMR) produces data on AMR annually, but there is a caveat that it collects data from tertiary care hospitals. The data presented in the report does not reflect the community levels of AMR in the country and should not be extrapolated to community settings,8. In contrast, the National Center for Disease Control (NCDC) published the data based on its 36 sentinel sites across the countries.9 Many laboratory information systems (LIS) are now available, but they come at a premium, which is a major limiting factor in most of the clinical microbiology laboratories in India. The second factor is the lack of local information technology systems capacity and human resources for implementation, inadequate support, and poor standardization.10 The NCDC, in its guidance document, mandated the use of WHONET for Data entry to its network hospitals under the National AMR Surveillance Network (NARS-Net).11
HOW TO USE WHONET IN AN INDIAN SET-UP?
The WHONET can be used differently for an Indian clinical microbiology laboratory.
To generate print out of Antimicrobial Susceptibility Test (AST) reports
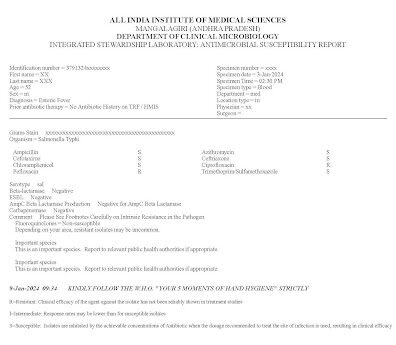
This friendly interface allows users to enter the susceptibility report in real-time and generate a printable AST report (Figure 2).
The laboratory may indicate which antibiotics should be included in the clinical report. The user may also specify “do not print” antibiotics or hide the antibiotics that it does not want to send to the clinician by “cascade reporting/tier-based reporting”. The laboratory also has the luxury to add features like methicillin-resistant Staphylococcus aureus (MRSA), inducible clindamycin resistance, extended-spectrum beta-lactamases (ESBL) producer, etc., in its report. In our experience, it takes hardly one minute to generate one report. The advantage of entering the data in real time, apart from developing the AST report, is the data gets stored simultaneously, and there is no backlog for data entry. It is of great help for laboratories that do manual reporting in a small or mid-level workload laboratory.
Use of BacLink for data entry
A laboratory with a high workload can use this approach.
For laboratories using Microsoft Excel-based register or Google sheet: For the laboratories that are now digitizing and upgrading to either MS Excel or Google Sheets register for their data entry, the same can be imported to WHONET format using the BacLink software. The tutorials for data conversion are available on the WHONET website.5
For laboratories using third-party LIS systems: For those laboratories with their own LIS in place, data can be exported to the WHONET by converting it to a comma-separated value (.csv) format and using BacLink.
For laboratories using automated ID/AST systems: Many manufacturers have built-in software to convert the data to a WHONET/BacLink compatible file.
Care should be taken that the WHONET configuration file and the BacLink files have the same variables; otherwise, there is a chance of data loss during the conversion. Also, it is of paramount importance that the data shall be entered in numerical form against each antibiotic and not “S, I & R” for susceptible, intermediate, and resistant, respectively. The data entry can be done weekly or monthly based on the sample load of that laboratory.
Making the antibiogram
An antibiogram is a periodic profile demonstrating microorganisms’ antimicrobial susceptibility within an institution/hospital. It aids clinicians in selecting the most appropriate empiric antibiotic therapy, monitoring the changes in resistance patterns of microorganisms and maintaining yearly records.12
Once the data is entered, the antibiogram can be made using the software’s data analysis tab following the steps mentioned below.
To launch the app, double-click the WHONET icon on the desktop.
Click “Open laboratory” after selecting the lab labelled “WHO Test Hospital.”
Click on the “Data analysis” button from the home screen of WHONET. A list will be generated.
Select “Data analysis” from this list. Once clicked on the button, the primary screen for WHONET analysis will appear. From this screen, command WHONET to perform the analysis of your choice.
Respond to the questions in the three areas on the left of the main analysis screen: analysis type, organisms, and data files.
Double-click on “Analysis type” and select “% RIS and test measurements.” Click on the “OK” button in the lower right corner.
Double-click on the “Organisms” key and select the major organism(s) needed for your analysis report. To select the organisms, double-click on its name. Using the search bar, analysis of individual microbes or whole species can also be done.
Double-click on “Data Files” – a window will open. Select “WHO-TST-2020. WHO-TST-2021,” and click “OK.” Make sure all required data files are filled before proceeding. Finally, click on “Begin Analysis.”
After the beginning of analysis, results will be generated in a new window.
LIMITATIONS OF WHONET
The far and foremost limiting factor of this amazing utility tool is that it works only on the Windows operating system. It also does not have a mobile application and is inoperable on mobile phones. While the WHONET is excellent for entry, analysis and reporting of resistant data, the software does not solve the purpose of a complete patient management system. In hospitals with existing patient management systems, the WHONET cannot be integrated, and the susceptibility data must be entered separately into WHONET either manually or through a BacLink. This would require an additional trained workforce for data entry and analysis. Although the program performs its task very well, in the long term, a surveillance system integrated with a patient management system might be more sustainable.
CONCLUSIONS
Indian laboratories should use WHONET. It does not have any financial burden. The only requirements for WHONET are a Windows computer system and basic computer knowledge. As most laboratories have at least one computer, installing the WHONET software is no longer an arduous job. It allows data to be entered in a real-time or staggered manner. The small laboratories can use it as a report-generating tool, while all the hospitals can use this software for generating their annual antibiogram. It helps in routine microbiology laboratory data management. It generates valuable information about antimicrobial susceptibility patterns over a place or time to provide the basis for and assess the effectiveness of prevention programs and policy decisions. If, on the national level, it is made compulsory to upload the data of WHONET monthly to all the hospitals and stand-alone laboratories to a repository (like it was done for tuberculosis), a true picture of antimicrobial resistance in the country would emerge. We need not extrapolate the data generated by a few tertiary care hospitals to the whole country as big and diverse as India.
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
REFERENCES
1- WHO. Antimicrobial resistance. Key facts. Geneva: World Health Organization. Accessed September 25, 2024. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
2- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629-55.
3- Aboushady AT, Sujan MJ, Pham K, et al. Key Recommendations for Antimicrobial Resistance Surveillance: Takeaways From the CAPTURA Project. Clin Infect Dis. 2023;77(Suppl 7):S581-7.
4. Simner PJ, Hindler JA, Bhowmick T, et al. What’s New in Antibiograms? Updating CLSI M39 Guidance with Current Trends. J Clin Microbiol. 2022;60(10):e0221021.
5. WHONET. The microbiology laboratory database software. Accessed September 25, 2024. https://whonet.org/
6. Agarwal A, Kapila K, Kumar S. WHONET Software for the Surveillance of Antimicrobial Susceptibility. Med J Armed Forces India. 2009;65(3):264-6.
7. O’Brien TF, Clark A, Peters R, Stelling J. Why surveillance of antimicrobial resistance needs to be automated and comprehensive. J Glob Antimicrob Resist. 2019;17:8-15.
8. ICMR. Annual Report. Antimicrobial Resistance Research and Surveillance Network. January 2022 to December 2022. New Delhi: Indian Council of Medical Research. Accessed September 25, 2024. https://main.icmr.nic.in/sites/default/files/upload_documents/AMRSN_Annual_Report_2022.pdf
9. NCDC. Annual Report. National Antimicrobial Surveillance Network (NARS-Net). January 2022 to December 2022. New Delhi: National Centre for Disease Control. Accessed September 25, 2024. https://ncdc.mohfw.gov.in/wp-content/uploads/2024/03/1257263841692628161.pdf
10. Turner P, Rupali P, Opintan JA, et al. Laboratory informatics capacity for effective antimicrobial resistance surveillance in resource-limited settings. Lancet Infect Dis. 2021;21(6):e170-4.
11. NCDC. Antimicrobial Resistance (AMR) Data Reporting using WHONET. National AMR Surveillance Network (NARS-Net). New Delhi: National Centre for Disease Control.
Accessed September 25, 2024. https://ncdc.mohfw.gov.in/wp-content/uploads/2024/03/82377282201681876947.pdf
12. Dikkatwar M, Vaghasiya J. Development and application of WHONET software in hospital antibiogram. Clin Epidemiol Glob Health. 2023;24:101424.
Submit a Manuscript:
Copyright © Author(s) 2024. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

