SASPI Ltd.
ASPICON-2024 PGIMER Abstracts
JASPI September 2024/ Volume 2/Issue 3 / Suppl. Issue
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract 001 ASPICON 2024 |August 22 -25 | 2024 |
Evaluation of Drug Use and Audit of Prescription of Restricted Antibiotics in the Intensive Care Unit of Tertiary Care Hospital
Manisha Aggarwal1*, Veenu Gupta1, Sandeep Kaushal2, Jyoti Choudhary1, P. L Gautum3, Rajesh Mahajan4
Department of Microbiology1, Department of Pharmacology2, Department of Critical Care3, Department of Medicine4, Dayanand Medical College & Hospital Ludhiana, Punjab, 141001, India.
* Presenting author: manisha903.doc@gmail.com
Background
Antimicrobial agents are the biggest contribution to the 20th century, which are used to prevent and cure infections. Reserve antibiotics are the last-choice of antibiotics to treat multidrug-resistant infections. The inappropriate use & irrational prescriptions of these drugs is a global health problem, and has an ill effect on health as well as on healthcare expenditure. To prevent it,regular and timely prescription audits are an important tool to improve the quality of healthcare.
Aim: To rationalize the overuse/misuse of the reserve drugs in intensive care units and to avoid emergence of drug resistance.
Material & Method
This was a cross-sectional observational study done in Dayanand Medical College and Hospital from March To May 2024 in patients admitted in ICUs.Inour hospital ReserveDrug policy six drugs were included: Linezolid, Polymyxin B, Colistin, Fosfomycin, Tigecycline&Ceftazidime- avibactam. The data was collected on reserve drug audit proforma. All the forms were analyzed by a team of Microbiologist, Pharmacologist and clinicians for the appropriate usage of the drugs on the basis of clinical condition, culture report and other investigations of the patient.
Result
Among the 272 prescriptions analyzed, 63.6% patients were males. Maximum number of reserve drugs were given to the patients belonging to the age group 61-80 years (41.5%). Audit report shows that most of the
reserve drugs were used in Medical wards & Colistin (124) and Tigecycline (91) were the most prescribed drugs. Single Restricted antimicrobial therapy was given in 66.5% patients, dual therapy in 25% and three drugs were given in 8.1%.Out of 272 Prescriptions of Restricted Antibiotics, 70.9% were found to be rational.
Conclusion
We can reduce the evolution of antibiotic resistance by its judicious use and education. So an audit is a mandatory exercise to provide quality care in the healthcare system.
|
Abstract 002 ASPICON 2024 |August 22 -25 | 2024 |
Investigation of a Cluster of Clostridioides Difficile Diarrhea in a Medical Oncology Unit
Sharmila Sengupta1*, Debasish Biswal1, Ananya Arora1, Vibha Mehta2, Rohit Garg2
Departments of Microbiology1, Infectious Diseases2, Amrita School of Medicine, Faridabad, 121002, India.
* Presenting author: sharmila.sengupta@fbd.amrita.edu
Background
The medical oncology unit of our tertiary care hospital experienced an increase in the number of Clostridioides difficile (C. difficile) infections from March 2024 to June 2024. This study aimed to investigate the rise in C.difficile cases, identify risk factors, and implement measures to contain and prevent future occurrences.
Methods
A comprehensive investigation involved collection from November 2022 to July 2024. The investigation included sample testing, analysis of infection trends across departments, and identification of risk factors such as outside hospitalization, multiple hospitalizations, prolonged hospital stays, antibiotic usage, infection control practices, and cleaning & disinfection protocols for environmental disinfection. Measures taken included strengthening hand hygiene, increasing the frequency of environmental cleaning, and introducing hydrogen peroxide fogging. Antibiotic stewardship programs were also reinforced, and active surveillance for new cases was implemented.
Results
The analysis revealed 34 positive cases out of C.difficile of 151 tested samples, with a 22.5% positivity rate. The majority of cases were concentrated in the Medical Oncology department (52%). Key risk factors identified included prior hospitalization (48%), multiple hospitalizations (72%), prolonged hospitalization (16%), and the use of high-risk antibiotics (76%). Environmental persistence of C. difficile spores and inadequate cleaning practices contributed to the outbreak. The implemented measures resulted in improved infection control, reduced antibiotic usage, and enhanced communication among staff.
Conclusion
The investigation highlighted critical risk factors and provided a basis for targeted interventions. Strengthening hand hygiene, optimizing environmental cleaning, and reinforcing antibiotic stewardship were effective in reducing the number of cases. Continued surveillance, staff education, and adherence to infection control protocols are essential to prevent future C.difficile in healthcare. The study underscores the importance of a multifaceted approach in managing healthcare-associated infections and enhancing patient safety.
Abstract 003 ASPICON 2024 |August 22 -25 | 2024 |
Changing Trends of Antibiotic Susceptibility Pattern in Escherichia coli Isolates Obtained from Urinary Tract Infections in a Tertiary Care Hospital in Sub-Himalayan Belt
Singh Gargi*, Sood Anuradha, Kaur Isampreet, Choudhary Anuradha
Dr. Rajendra Prasad Government Medical College, Kangra at Tanda, Himachal Pradesh, 176002, India.
* Presenting author: udayjosan0797@gmail.com
Background
Escherichia coli is the most common organism causing both communities as well as hospital-acquired UTIs. The effectiveness of antibiotics used to treat these infections is threatened by growing bacterial resistance.
Aim & Objectives: This study aims to analyze the changing trends in the antibiotic susceptibility pattern of Escherichia coli isolates obtained from UTI cases in the last three years.
Methodology
Retrospective data analysis of antibiotic susceptibility pattern in Escherichia coli obtained between Jan 2021 -Dec 2023 in the Department of Microbiology.
Results
A total of 22,802 urine samples were tested over three years. In 2021, a total of 457 isolates of E.coli were obtained followed by 1072 in 2022 and 977 in 2023.. Maximum isolates were obtained in the age group of 18-45 years. Amongst the most commonly used urinary antibiotics, Nitrofurantoin showed a declining trend in susceptibility ranging from 93%in 2021 to 76% in 2022 and 51% in 2023. Fosfomycin showed steady susceptibility rates in 2021 (96%), 2022 (96%), and 2023 (94%). Ciprofloxacin showed a decrease in susceptibility rangingfrom40%in 2021 and 32% in 2023. Piperacillin showed a sharp decline in susceptibility rates from 84% in 2021,74% in 2022 and 20% in 2023. Ampicillin showed a decrease in susceptibility from 30% in 2021 to 25% in 2023.
Conclusion
An increasing trend in resistance to common urinary antibiotics like nitrofurantoin, Cephalosporins, and Fluoroquinolones emphasizes the need to strengthen hospital infection control practices and judicious use of antibiotics for empirical therapy according to standard guidelines. This can further help in the effective implementation of AMSP guidelines, guiding empirical treatment, and formulating hospital antibiotic policy according to local antibiograms.
Abstract 004 ASPICON 2024 |August 22 -25 | 2024 |
Barriers and Facilitators of Outpatient Parenteral Antimicrobial Therapy Practice and its Role in Antimicrobial Stewardship – A Pilot Longitudinal Study
Amit Kumar Mathur*, Prasan Kumar Panda, Ravi Kant, VS Pai, Mukesh Bairwa, Darab Singh, Nilanjana
Department of Internal Medicine (ID Division), All India Institute of Medical Sciences (AIIMS), Rishikesh, 249203, India.
* Presenting author: ak668659@gmail.com
Introduction
Outpatient parenteral antimicrobial therapy (OPAT) offers a crucial method for administering IV/IM antimicrobials outside hospitals, enabling patients to complete treatment safely outside and many hospital-acquired events. This pilot study evaluates real-world barriers and facilitators of OPAT’s practice in resource-poor settings, emphasizing its role in antimicrobial stewardship.
Methodology
This pilot longitudinal observational study included patients meeting OPAT checklist criteria and committed to post-discharge follow-up. Pre-discharge demographic data noted. Various barriers and facilitators were identified after an extensive literature review by preparing a fishbone diagram, data collection and analysis, and patient feedback.
Results
The mean age of patients was 38 years [Range=21-63], with Male-14 and Female-4, with all OPAT administered at the home by family members on 7/18, and by a local nurse on 11/18. Infections requiring OPAT were Typhoid-5, UTI-4, HAP-4, Meningitis-3, IE-1 and multiple visceral abscess-1. 17/18 patients became afebrile and one instance of prematurely discontinued OPAT regimens and one readmission was observed. Additionally, one patient developed thrombophlebitis. No education, counseling, or demonstrations were done before discharge in almost half of the patients. It saves 2 week’s duration of hospitalization For identifying potential problems, a fishbone diagram tailored to OPAT [Barriers (red) and Facilitators (green) was prepared (Fig 1).
Conclusion
This pilot study provides a comprehensive understanding of barriers and facilitators influencing OPAT practices in a resource-poor setting. By addressing these barriers and leveraging facilitators, each healthcare facility can optimize OPAT delivery, improve patient outcomes, and ensure a more efficient and patient-centered approach to antimicrobial therapy. OPAT reduces hospital stays and hospital-acquired infections, is crucial in combating antimicrobial resistance (AMR), and thus directly contributes to integrated antimicrobial stewardship, aligning with a global action plan for AMR in infection prevention and antimicrobial optimal utilization.
Abstract 005 ASPICON 2024 |August 22 -25 | 2024 |
Development and Characterization of A. Annua L. Whole Leaf Extract Loaded HSA Nanoparticles Using QbD Approach: A Novel and Potential Antimalarial Formulation
Anuradha Mishra*, M. Z. Abdin
Centre for Transgenic Plant Development, Department of Biotechnology, School of Chemical and Life Sciences, Jamia Hamdard, New Delhi, 110062, India.
* Presenting author: mishra.9419@gmail.com
Background
Malaria, caused by Plasmodium protozoa, remains a major global health issue. Significant efforts have been made to eradicate malaria, with chemotherapy being a key strategy in combating the disease. The most significant antimalarial drugs are artemisinin (ART) and its semi-synthetic derivatives, which have been used in combination therapy (ACTs) for improved efficacy. However, despite early success, ACTs have proven unsuccessful in many endemic nations due to drug resistance. The development of nano drug delivery systems (NDDSs) is critical to overcoming this challenge and improving treatment outcomes.
Methods
This study aimed to design, optimize, and develop Artemisia annua L. whole leaf extract-loaded human serum albumin (HSA) nanoparticles using a quality-based design (QbD) and risk assessment methodology. The nanoparticles were synthesized via the desolvation method and characterized by dynamic light scattering (DLS), transmission electron microscopy (TEM), scanning electron microscopy (SEM), and Fourier-transform infrared spectroscopy (FT-IR).
Results
The optimized nanoparticles exhibited a particle size of 84.73 nm, a polydispersity index (PDI) of 0.23, a zeta potential of -22.11 mV, and an entrapment efficiency exceeding 90%. Additionally, the ART release profile demonstrated sustained release and stability studies indicated long-term stability.
Conclusion
The A. annua L. whole leaf extract-loaded HSA nanoparticles developed in this study present a promising antimalarial drug delivery system. The developed nanoparticles may have the potential to improve treatment outcomes and overcome drug resistance, thereby addressing a critical need in the fight against malaria.
Abstract 006 ASPICON 2024 |August 22 -25 | 2024 |
Implementing Antimicrobial Prescription Checklist to Improve Antimicrobial Prescription Quality – A Pilot Project Towards Antimicrobial Stewardship
Pratip Das*, Nitin Gaikwad, Meenalotchini P Gurunthalingam
Department of Pharmacology, All India Institute of Medical Sciences, Raipur – 492099 (Chhattisgarh), India.
* Presenting author: pratipdas477@gmail.com
Background
Inappropriate use of antimicrobials is a major cause of antimicrobial resistance (AMR). Antimicrobial Stewardship (AMS) interventions are required to curtail the AMR. The antimicrobial prescription of an indoor patient is an important target for AMS intervention. Enhancing the quality of antimicrobial prescriptions will help ensure that antimicrobials are used appropriately.
Objective: To assess the improvement in the quality of antimicrobial prescription against the ‘Antimicrobial Prescription Checklist’ and the effect of improved antimicrobial prescription practices on various clinical outcomes.
Methodology
Active surveillance was conducted in a randomly selected ward of the General Medicine department for two months. Prescription data was recorded daily using a pre-validated Data Abstraction form. Patients who received antimicrobial agents via systemic route were included for analysis. Patient days were counted daily at 6 pm for calculating days of therapy (DOT) per 1000 patient-days (PD). The ‘Antimicrobial Prescription Checklist (APC)’ was used to ensure compliance with antimicrobial prescriptions. Data was collected before and after the intervention. The educational intervention for antimicrobial stewardship included didactic lectures, small-group discussions, WhatsApp notifications, and posters in the ward. Data was analyzed for APC criteria indicators, clinical outcomes like DOT per 1000 PD, WHO prescribing indicators, antimicrobial therapy duration, and length of stay.
Results
The educational intervention received positive and immediate feedback from the prescribers. A slight improvement in a few APC criteria, including the notation of ‘review after 48 hours’, the day of antimicrobial prescribed, and the report of culture sensitivity was observed. The average number of antimicrobials prescribed per hospitalization (2.36 vs 1.9) and the average duration of antimicrobial treatment days (12.53 vs 8.1) were decreased. A decreased consumption (per 1000 PD) of ‘Watch’ group antimicrobials (Meropenem: 171 vs 41; Piperacillin-tazobactam: 264 vs 192; Vancomycin: 90 vs 12) was observed. The median length of antimicrobial therapy (629 vs 383 days) and hospital stays [10 (IQR:7 – 18) vs 9 (IQR: 6 – 13) days] was decreased.
Conclusion
The APC Criteria can improve prescription quality and identify key antimicrobial stewardship areas. The educational intervention improved clinical outcomes. However, sustainable and long-term observations are needed to draw a meaningful conclusion.
Abstract 007 ASPICON 2024 |August 22 -25 | 2024 |
Phenotypic and Genotypic Characterization of Carbapenem-Resistant Enterobactarales Obtained from Various Clinical Specimens
Vipasha*, Narinder Kaur , Shahbaz Aman
Department of Microbiology, MMIMSR, Maharishi Markandeshwar [Deemed to be University], Ambala, Haryana, India.
* Presenting author: vipkaushal12@gmail.com
Background
The rise of Carbapenem-resistant Enterobacterales (CRE) presents a significant threat to global health, particularly due to the production of carbapenemase enzymes, including New Delhi Metallo-β-lactamase (NDM-1).
Methodology
The study investigates the prevalence and phenotypic detection of carbapenemase-producing Enterobacteriaceae (CRE) in clinical specimens, emphasizing the distribution of the NDM-1 gene among carbapenem-resistant isolates.
Result
A total of 17,984 clinical specimens were analyzed, with 1,843 culture-positive samples revealing Gram-positive cocci (GPC) in 632 cases, Gram-negative bacilli (GNB) in 1,207 cases, and Candida albicans in 4 cases. Among Enterobacterales, Escherichia coli was the most common isolate (666), followed by Klebsiella species (172), Citrobacter species (93), and others. Phenotypic detection of carbapenemase production was done by employing modified Carba NP, Rapidec Carba NP, EDTA combined disc assay, modified Hodge test, and modified carbapenem inactivation assay. The study found significant variability in detection rates among these methods. The Modified Carba NP and Rapidec Carba NP tests showed a higher sensitivity for detecting carbapenemase production compared to other methods. Among the 150 CRE isolates, 68 were identified as NDM-1 gene carriers, predominantly in E. coli (33) and Klebsiella species (29).
Conclusion
The findings underscore the need for comprehensive phenotypic and genotypic testing to accurately identify and manage CRE infections, thereby aiding in the implementation of effective infection control measures.
Abstract 008 ASPICON 2024 |August 22 -25 | 2024 |
Real-time Assessment of the Effectiveness of Alcohol-based Hand Rubs in Disinfecting Non-critical Patient Care Items in Tertiary Care Hospital Settings
Divya Darshan Panigrahi*, Nithin Varghese, Shalini Mann,, Priyanka Singh, Mansi Gupta, Ujjwala Gaikwad
Department of Microbiology, All India Institute of Medical Sciences, Raipur – 492099 (Chhattisgarh), India.
* Presenting author: divyadarshanpanigrahi2002@gmail.com
Introduction
Non-critical patient care items are frequently implicated in the transmission of Multi-drug resistant organisms (MDROs), resulting in hospital outbreaks. Alcohols are the most preferred agents for disinfection of these items due to their rapid action and compatibility with the majority of hard surfaces. Many hospitals use ‘alcohol-based hand rubs’ (ABHR) for this purpose due to their easy availability, even though they are designed for skin antisepsis and not hard surface disinfection. This study assessed the effectiveness of ABHR in disinfecting them, in real-time situations, as little is known about it.
Methodology
A cross-sectional study for two months was conducted in the inpatient facility of a 1,000-bed tertiary care hospital. Approximately 210 patient care items were sampled from various ICU and non-ICU locations. Two samples from each equipment were collected, one before and one after disinfection by ABHR, while the equipment was in real-time use. The collected samples were processed for aerobic colony count. Mean CFU/ml of bacteria grown from pre and post-disinfection sampling was compared to determine the efficacy of the disinfection procedure.
Results
The baseline contamination rate for the items was observed to be 72.4% (152/210) which was higher in non-ICU locations than in ICUs. Most of the items (96.1%) were contaminated with Coagulase Negative Staphylococcus. The effectiveness of ABHR in decontaminating patient care items was found to be 93.1% ± 6.3. ABHR was also found to be effective in decontaminating objects with an MDRO microbial profile; however, objects contaminated with Staphylococcus aureus were the least effectively removed by it.
Conclusion
ABHR was found effective for the disinfection of non-critical patient care items in real-time scenarios including its action on MDROs. Hence, it can be safely used to achieve the disinfection of hard surfaces in addition to its recommended use.
Abstract 009 ASPICON 2024 |August 22 -25 | 2024 |
A Cross-sectional, Qualitative, and Observational Study was Conducted in the OPD Setting of a Rural and an Urban Setting Community Hospital
Rashmi Surial*, Chetan Chandel
Society for Health Information Systems Programmes (HISP India), New Delhi, India
* Presenting author: rashmi.surial@hispindia.org
Introduction
The overuse and misuse of antimicrobials in human health with other contributing factors like inappropriate prescriptions, prolonged use of antimicrobials, and sometimes the presence of bacteria in the environment and entry of these antimicrobials to the food chain through any means have increased the development and spread of AMR globally.
Methodology
This study is a cross-sectional, prospective, and observational study conducted in an outpatient department (OPD) of two community health settings (rural and urban). The main objective of the study is to evaluate the antibiotic prescription pattern in an OPD setting. Using a random sampling procedure, 1724 prescriptions were studied from an urban setting and 1151 from a rural setting.
Results
Some of the WHO core indicators were studied and it was seen that 98% of the prescriptions were from the essential drug list(EDL) in a rural setting and 87% were from an urban setting. 99% of the prescriptions were based on generic names in an urban setting and rural areas it was around 91%. 15.25% of prescriptions from urban settings were based on diagnosis. The most prescribed antibiotic from an urban setting was Cefixime, whereas, from a rural setting, it was Amoxyclav. Most of the cases reported from this setting were from general medicine OPD, whereas in rural settings it was from dental OPD where the antibiotics were prescribed just in case.
Conclusion
We see high use of antibiotics from the Watch group being prescribed in urban settings, whereas in the rural setting, it is from the Access group. But on the positive side, we saw most of the prescriptions in both settings were made from the essential drug list and most of them were written by generic names following the WHO guidelines. Making these prescription patterns available will help clinicians in studying the current practicing scenario.
Abstract 010 ASPICON 2024 |August 22 -25 | 2024 |
A Study to Evaluate the Use of Antimicrobial Agents in Patients of Burns at a Tertiary Care Hospital.
Harshil Damor*, Anuradha Gandhi, Vishal Mishra, Chetna Desai
Department of Pharmacology, B.J Medical College, Ahmedabad, Gujarat, 380016, India.
* Presenting author: harshil.damor@gmail.com
Introduction
Burns are the most painful of all injuries and a major global public health problem. Mortality due to sepsis is a major concern which can be prevented with proper antimicrobial agents according to culture sensitivity.
Methodology
This prospective, observational study was conducted on 104 adults who were having burns and were admitted at Civil Hospital, Ahmedabad. After approval from the Institutional Ethics Committee, each patient was followed up daily for the first seven days and then weekly till discharge. Demographic details, vitals, local wound examination, numeric pain rating scale, culture sensitivity report, drug treatment, and adverse events were recorded and analyzed using appropriate statistical tests.
Results
A total of 104 adult burn patients were enrolled. Male to female ratio was 1:1.89. At the time of admission the mean total body surface area (TBSA) burned was 24 + 16%. The most common type of burn was thermal burns(45.19%). Patients who suffered from severe full-thickness burns were 73(70.19%). The most commonly used topical antimicrobial was Silver sulfadiazine (100%) while Systemic antibiotics like amoxicillin + clavulanic acid (99%) was used empirically and prophylactically in 82 and 22 patients respectively. In addition to these Piperacillin tazobactam(18.27%), Linezolid(35.58%), Metronidazole(14.42%) were used as add on therapy. Culture sensitivity is done in 23(22.11%) patients among them 7 (30.43%) Pseudomonas aeruginosa, 4(17.39%) Acinetobacter baumannii, and 4(17.39%) staphylococcus aureus isolated. 64 patients were discharged with healing wounds. The total reported adverse drug reactions were 31 among them 15(48.39%) were constipation. The mean length of hospital stay was 21 + 15 days. Overall mortality observed due to sepsis is 7(33%).
Conclusion
The extent of the burn area, days of hospital stay, and nature of the burn are the risk factors for the development of infection. Antimicrobials based on culture sensitivity reports can prevent infection-related mortality. Public awareness about burns prevention is also advisable.
Abstract 011 ASPICON 2024 |August 22 -25 | 2024 |
A Point Prevalence Survey Study (PPS) of Antimicrobial Consumption in a Tertiary Care Super-speciality Hospital of West Bengal from 2021: Some Interesting Findings
Raja Chakraverty1*, Kalyan Samanta2
Department of Critical Care Medicine1, Department of Pharmacology2, Institute of Post Graduate Medical Education and Research, Kolkata, 700020, India.
* Presenting author: rchakraborty20@yahoo.com
Background
The burden of antimicrobial resistance (AMR) is an emerging global health issue. Resistance occurs when bacteria, parasites, viruses, or fungi are exposed to antimicrobials but not killed by them. The study was conducted in the year 2021 to gather baseline information and to assess the antimicrobial consumption practices across six departments in a tertiary care super specialty hospital in West Bengal.
Methodology
The institutional ethics committee accorded the study protocol. A modified version of a patient data collection form proposed by Global PPS was developed on Epi Info software version 7 (CDC). Data of all patients admitted to a ward at 08.00 am data were studied. The use of antimicrobials was categorized as empiric, prophylactic, or lab-based. WHO-AWARE classification of antimicrobials was instituted for categorizing usage.
Results
A total of 85 patient-related data was collected in the designated survey form. The total number of beds covered was 340 and the number of patients on antimicrobials was found to be low at 21.27 %. The patients surveyed were predominantly female (78.8 %). The mean number of antimicrobials per patient was found to be 1.62 (range of 1.4 to 2.2) Relatively low number of patients were found to be on 2 or more antimicrobials. Double gram-negative and Double anaerobic coverage of AM used varied across departments covered in the survey.
Conclusion
Our point prevalence study was able to facilitate the conducting of a point prevalence survey in a high patient volume tertiary care hospital with a paper-based medical record system and depicted the baseline parameters of intervention for instituting future action and policy changes.
Abstract 012 ASPICON 2024 |August 22 -25 | 2024 |
Normal Cytology Doesn’t Preclude High-risk HPV Infection
Priyal Gupta1*, Ajay halder2, K. Pushpalatha2, Shashank Purwar1
Departments of Microbiology1, Department of Obstetrics and Gynaecology2, All India Institute of Medical Sciences, Bhopal, 462020, India.
* Presenting author: priyal.phd2019@aiimsbhopal.edu.in
Abstract
Human papillomavirus infection is the major risk factor for cervical cancer. Infection with certain high-risk HPVs makes an individual more prone to develop cancer. Therefore, understanding the prevalence and distribution of HPV genotypes is necessary to implement targeted prevention strategies. Hence, in this study, we evaluated the burden and distribution of HPV genotypes among women across the cervical cytological changes. 125 symptomatic women were recruited in the following three groups; women with a) cervical cancer, b) squamous intraepithelial lesions, and c) normal cytology based on the Pap test. We evaluated the presence of HPV and its genotypes using RT-PCR with a 16/18 genotyping kit. The overall prevalence of HPV infection was observed to be (84/124) 67.2%. Prevalence of HPV infection in cervical cancer cases was highest with (48/50) 96% positivity followed by 56% and 44% among women with squamous intraepithelial lesions and normal cytology respectively. HPV 16 emerged as the predominant genotype, accounting for 59.60% of cases. Following closely, HPV 18 exhibited 8.33% positivity. HPV 8 GTS genotype demonstrated 17.85% positivity, suggesting the presence of any of the following genotypes: 31, 33, 35, 51, 52, 56, 58, or 66. Multiple genotypes coexisted in 4.76% of patients. Conclusively, our finding indicates HPV 16 to be the most common genotype followed by HPV 8 GTS. This study reflects the need to screen symptomatic women for HPV even if their pap test suggests normal cytology for early identification and monitoring of women infected with high-risk HPV.
|
Abstract 013 ASPICON 2024 |August 22 -25 | 2024 |
Cognizance on Antimicrobial Stewardship Indicators in Intensive Care Unit
Ramya Rajendran*, Manisha Subarao Mane, Syeda Saba Hashmiya
ESIC medical college and hospital, Sanathnagar, Hyderabad, Telangana 500038, India.
* Presenting author: ramyanysha19081996@gmail.com
Background
Antimicrobial resistance (AMR), is recognized as one of the top ten public health threats by the World Health Organization. About 4.95 million deaths were associated with bacterial AMR globally. Fighting antimicrobial resistance requires appropriate diagnosis and monitoring of the use of antibiotics through an effective Antimicrobial stewardship program which assists in monitoring antibiotic resistance trends, antimicrobial consumption, and clinical outcomes of patients in healthcare facilities.
Methodology
ICU WORKUP: Regular visits were made to the ICU and the patient’s relevant data were collected including Dose, duration, blood culture practices, and course of antimicrobials given.
LAB WORKUP: Direct smear from the flagged blood culture was processed further along with Antibiotic susceptibility testing and the outcome and process indicators of AMSP were calculated accordingly.
Results
The demographic parameters of the patients revealed that the number of males admitted to the ICU was almost equal to that of females and the median age of patients was around 46.5 years. The mortality rate in this study was found to be 36.5 %. In our study, we analyzed the utilization patterns of Antimicrobial agents in terms of DDD/100 patient days and DOT/100 patient days. The median DOT/100 patient days was 7 (0–29). The most commonly used antibiotics are Meropenem, Piperacillin-tazobactam, Ceftriaxone, and Azithromycin with DDDs 1.45, 3, 6, and 3 respectively. Appropriate timing of Blood culture collection was followed in 70% of the cases,30% of cases were already started on empirical therapy before sending samples for culture. The infection-specific mortality was found to be 12.1% while the infection-specific length of stay was increased in 3 patients by 10 days and antibiotic-associated diarrhea was not seen during the study period.
Conclusion
In conclusion, our study reveals that antimicrobials are widely prescribed in critically ill patients which forms a significant proportion of the total drugs consumed in the ICU. Decision-making by the clinicians can be optimized which will result in good treatment compliance since the patients will be exposed to fewer and more appropriate antibiotics.
Abstract 014 ASPICON 2024 |August 22 -25 | 2024 |
Antimicrobial Stewardship: A Tertiary Care Experience
Mahadevan Kumar*, Vrushali Thakar, Deepa Devhare, Shraddha Paralkar, Ayana Jain
Department of Microbiology, Bharati Vidyapeeth (DU) Medical College and Hospital Pune, 411 043, Maharashtra, India.
* Presenting author: dr.mkumarmicro@outlook.com
Background
Antimicrobial resistance (AMR) is a global health concern. An antimicrobial stewardship program is the core strategy to tackle AMR. The goals of this program are to rationalize prescribing and avoid unnecessary use of antimicrobials. It plays a significant role in decreasing the incidence of resistance, reducing the development of multidrug-resistant organisms, and improving patient care with the long-term goal of preserving antimicrobials.
Methodology
The antimicrobial stewardship program was started in 2019 at our tertiary care center. This ongoing program includes microbiology, the infection control department, infectious disease physicians, and clinical pharmacists. The data is collected on data forms which are then collated on Microsoft Excel. The team provides stewardship advice based on the hospital antibiotic policy and the results of the culture.
Results
The total no. of patients admitted to the hospital for the period 2022-2023 was 85833. Of these, the percentage of patients administered antimicrobials varied from 8.1% to 25.5% per month with an average of 16%. Compliance with stewardship advice was around 78%. The percentage of compliance with de-escalation advice was 74.4%. The combined Duration of Therapy for all antimicrobials per 1000 patient days was 474. DOT per 1000 patient days for selected antimicrobials was as follows: Piperacillin-tazobactam (53.7), Carbapenems (49.5), Polymyxins (13.1), First-generation Cephalosporins (31.5), Third-generation Cephalosporins (78.5), Vancomycin (9.8) and Fluoroquinolones (6.4). Consumption of selected antimicrobials in DDD per 1000 patient days was as follows: First-generation Cephalosporins (32.6), Third generation Cephalosporins (72.3), Piperacillin-tazobactam (40) Carbapenem (30) Polymyxin (3), Vancomycin (4.7). The Length of Therapy of antimicrobials per 1000 patient days has ranged from 146 to 322 days with an average of 220 days. The average length of stay of the patients on antimicrobials was 9.3 days. The average cost per patient per day was Rs. 485.
Conclusion
The implementation of the Antimicrobial Stewardship Program at our center has resulted in the rationalization of antibiotic prescriptions as compared to other institutions of a similar nature.
Abstract 015 ASPICON 2024 |August 22 -25 | 2024 |
Drug Resistance Profile of TB Patients Attending a Tertiary Care Centre in the Northern Region of India
Kanchan Dochania1*, Sunil Dhatwalia1, Rakesh Yadav1, A.N. Aggarwal2, Rajesh Rana3 , Sunil Sethi1
Department of Medical Microbiology1, Department of Pulmonary Medicine2, State TB cell Officer3, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, 160012, India.
* Presenting author: 1205kanchan@gmail.com
Background
The emergence of multidrug-resistant MDR-TB and extensively drug-resistant XDR-TB are serious threats to global TB control. Molecular tests like GenoType MTBDRplus have revolutionized MDR-TB diagnosis by rapid detection of resistance, leading to early and appropriate management of DR-TB. Retrospective data was collected to determine the study drug-resistant pattern among TB patients.
Methodology
A retrospective analysis was done over 12 months from January 2023 to December 2023 to study the resistance pattern and mutations present in DR-TB in adults with suspected pulmonary or extrapulmonary tuberculosis using Hain’s GenoType MTBDRplus VER 2.0.
Results
Over 12 months, samples from 6425 patients with suspected TB were received, 822 out of these 6,425 isolated were tested for drug resistance by Hain’s GenoType MTBDRplus VER 2.0. 11.68% (751) were sensitive to isoniazid and rifampicin while 8.63% were DR-TB (71 out of 822). Out of these 71, 20 were MDR TB, 48 were isoniazid monoresistant (0.74%) and 3 were rifampicin monoresistant. Out of 3,726 males, 511 were tested for drug resistance; 9.00% (46 out of 511) were resistant, and out of 2,633 females; 314 were tested for drug resistance; 9.23% were resistant (29 out of 314).
Conclusion
We cannot solely rely on Xpert MTB/Rif Assay for detection of drug resistance due to the risk of missing reducing turnaround time and leading to early management of DR-TB cases.
Abstract 016 ASPICON 2024 |August 22 -25 | 2024 |
Targeted Pharmacovigilance for Metronidazole-Induce Neuropathy in Patients of Amoebic Liver Abscess at A Tertiary Care Hospital: An Ambispective Study
Gulam Gouse1, Puneet Dhamija2, Bhupinder Solanki2*, Shazia Hasan2, Intezaar Ahmed2, Rohit Gupta2, Ravi Kant2, Farhan-ul-Huda2
Department of Pharmacology, School of Pharmaceutical Sciences and Technology, Sardar Bhagwan Singh University, Dehradun, 248161, India.
All India Institute of Medical Science India, Rishikesh, 249203, India.
* Presenting author: bhupindersolanki83@gmail.com
Introduction
Metronidazole has been the front-line choice for several anaerobic and protozoan infections worldwide (1). Metronidazole is widely prescribed and recognized for its effectiveness in treating various infections, including amoebic liver abscesses (ALA). However, its use comes with potential complications, particularly the development of neuropathy, which affects the nerves and can cause significant discomfort and impairment for patients (2). While existing knowledge suggests that neuropathy is a rare side effect, the exact incidence rates and risk factors remain areas of ongoing research. Our study addresses the neuropathy risk associated with metronidazole treatment for ALA. To assess the incidence and severity of metronidazole-induced neuropathy in patients with ALA managed with Metronidazole.
Methodology
It was an observational study conducted in the Department of General Medicine, General Surgery, Gastro-Enterology, Paediatric Surgery, and Pharmacology, All India Institute of Medical Sciences, Rishikesh, UK, India. The duration of the study was six months. All patients diagnosed with ALA managed with Metronidazole were included (Adult and pediatric above 5 years and patients from both genders). The suspected adverse drug reaction reporting form, version 1.4, was used to collect data. All the suspected cases of adverse events were reported to the ADR Monitoring Centre, AIIMS, Rishikesh. The causal relationship was established by the standardized WHO UMC Causality Assessment. The analyzed data was then uploaded to Vigiflow software and sent to NCC. The severity and preventability of metronidazole-induced neuropathy were assessed using the Modified Hartwig severity assessment scale and Modified Schumock-Thornton Scale, respectively. Retrospectively, adverse drug reaction (ADR) data were collected from Vigiflow software at AMC, AIIMS, and Rishikesh and cross-checked with the respective department, treating physicians, and Patients (telephonically) for further information.
Results
A total of 165 patients were recruited. 23 developed neuropathies, primarily due to long-term medication use and risk factors like alcohol, tobacco, and diabetes. Most affected were males (69%) within the 20-50 age range. The occurrence of neuropathy symptoms was most frequently reported with the 800 mg dose. The most common duration of Metronidazole use was 30 days. 26% of patients suffered from severe symptoms of metronidazole-induced neuropathy.
Conclusion
This study identified the percentage of patients developing neuropathy after metronidazole use in ALA, including gender, age, severity, dose, and duration of treatment. Awareness of the drug’s potential for neurotoxic effects is crucial, and its use should be judiciously managed to prevent unnecessary exposure. These data will be helpful for the risk minimization and risk management plans.
Abstract 017 ASPICON 2024 |August 22 -25 | 2024 |
A Comparative Study to Assess Sputum and Bronchoalveolar Lavage ( BAL) Sample in Infective Lung Diseases
Sonali Bhattar1*, Shikhar Saxena2, Tulika Choudhary3, Vikas Dogra4
1- Department of Microbiology, Institute of Human Behaviour & Allied Sciences Delhi, India.
2- Department of Microbiology, Rajiv Gandhi Superspeciality Hospital, Delhi,,India.
3- Department of Microbiology; Rama Medical College Hospital and Research Centre Hapur,, India.
4- Department of Pulmonology, Rajiv Gandhi Superspeciality Hospital, Delhi2.
* Presenting author: drsonalivds1@gmail.com
Introduction
Establishing the causative pathogen early in infective lung diseases is cardinal for reducing diagnostic delay and ensuring the administration of effective antibiotics, especially in an era of growing antibiotic resistance, and will decrease mortality and morbidity.
Aims & Objectives: This study aims to analyze concordance or discordance among sputum and BAL samples.
Methodology
This retrospective study was conducted in a tertiary hospital in North India from January 2022 to December 2022 and a total of 3758 sputum samples and 253 BAL samples were received. Samples were directly inoculated on Blood agar, Chocolate agar, and MacConkey agar. Confirmation of isolates and antimicrobial susceptibility testing was done with the help of an automated system (VITEK 2@bioMerieux). These samples were analyzed for concordance amongst 56 samples for which both BAL and sputum were sent in close succession to rule out other infection incidence.
Results
Concordance among various microorganisms isolated from BAL and Sputum samples was observed in about 80 % of cases which indicates that sputum samples may be used in cases where BAL samples cannot be taken.
Conclusion
Sputum analysis is a more cost-effective and noninvasive sampling method. This study can be further used prospectively with clinicians to de-escalate antibiotics if started, and/or to change antibiotic therapy according to the sputum sample culture results.
Abstract 018 ASPICON 2024 |August 22 -25 | 2024 |
Phage Selection Can Restore Antibiotic Sensitivity to Treat Urinary Tract Infections: Preclinical Study Findings
Naveen Chaudhary*, Harpreet Kaur, Dharmendra Singh, Ravi Kumar Maurya, Vinay Modgil, Balvinder Mohan, Neelam Taneja
Department of Medical Microbiology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, 160012, India.
* Presenting author: Chaudharynaveen.999@gmail.com
Background
Phage-antibiotic synergy (PAS) has emerged in recent years to possibly replace or supplement traditional antibiotic therapy. Here, we report a unique mechanism involved in the effectiveness of phage PGN80A and antibiotics combination against multidrug-resistant uropathogenic Escherichia coli isolates.
Material & Methodology
To unravel the pharmacological dynamics, we employed whole genome sequencing for wild-type isolates and phage PGN80A-resistant variants (n=10) using NovaSeq6000. To determine the PAS in phage PGN80A (102 -109 PFU/mL) five different classes of antibiotics with varied concentrations (1–512 μg/ml) were co-cultured with bacterial culture. To examine the role of cell filamentation in synergism, we examined the morphology of wild and mutant bacterial isolates using scanning electron microscopy. A transurethral catheter mice model was used to test and compare the efficacy of phage and antibiotic synergy.
Results
In our pharmacogenomic analysis, we revealed that phage-resistant variants acquired multiple single nucleotides (n=3868) and frameshift mutations (n=184). Cells were significantly shorter for bacteria grown in a Trypticase soy broth without imipenem compared to those grown in a medium with the sub-inhibitory concentration of imipenem and low titer of phage PGN80A. Phage 80A demonstrated a pharmacologically relevant synergistic effect in combination with imipenem at 1/100 of the MIC concentration. A significant reduction (p<0.01) in bacterial load was observed in mice treated with phage PGN80A (106 PFU/ml) and a low dose (25 mg/kg) of imipenem.
Conclusion
Our study undertakes a pharmacologically oriented comprehensive analysis of phage-antibiotic interactions for scrutinizing synergy, additivity, and antagonism. We observed morphological changes after antibiotic application, the occurrence of multiple mutations in phage-resistant variants indicating the involvement of multi-antibacterial strategies. We conclude that phages, such as PGN80A, represent a new approach to traditional therapeutics where phages exert selection for MDR bacteria to become increasingly sensitive to conventional antibiotics.
|
Abstract 019 ASPICON 2024 |August 22 -25 | 2024 |
Evaluation of Antimicrobial Drug Promotional Literature: A Critical Analysis Using Diverse Standard Tools
Ankush Goyal*, Puneet Kaur, Jasmeen, Navjot Kaur, Ranjana , Jasbir Singh
Department of Pharmacology, Government Medical College, Patiala, 147001, Punjab, India.
* Presenting author: ankush8121996@gmail.com
Background
Drug promotional literature (DPLs) are known to influence the drug prescribing practices of physicians. Previous studies in multiple therapeutic areas have often shown that the DPLs lack fair balance, manipulate data, and make unsubstantiated claims. There is a paucity of research on critical appraisal of antimicrobial DPLs in particular. This could lead to irrational prescribing patterns of antibiotics thereby exacerbating antimicrobial resistance. Therefore, the current study is planned to assess the compliance of antimicrobial DPLs to various standard guidelines.
Material & Methodology
A cross-sectional observational study was conducted over three months to analyze antimicrobial DPLs. These were collected from multiple sources including various clinical departments of our hospital, medical representatives, and nearby pharmacy outlets. Institute Ethics Committee approval was not sought as the utilized information was available in the public domain. DPLs were evaluated using multiple criteria such as WHO Ethical Criteria for Medicinal Drug Promotion, International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) Code of Practice, Uniform Code for Pharmaceuticals Marketing Practices (UCPMP), Organization of Pharmaceutical Producers of India (OPPI) and Association of British Pharmaceutical Industry (ABPI) code of practice. In addition, the “Fair balance” of DPL information was assessed using USFDA criteria. Data were entered in a Microsoft Excel sheet and analyzed using descriptive statistics.
Results
The majority of DPLs did not comply with the standard guidelines completely and lacked a fair balance of the information. Reference to scientific literature substantiating claims was not provided in most of the studied DPLs.
Conclusion
The study provided valuable insights into the quality of antimicrobial DPLs. Regulatory measures are needed to ensure healthcare professionals receive accurate, current, unbiased evidence-based information on antimicrobials for rational prescribing.
Abstract 020 ASPICON 2024 |August 22 -25 | 2024 |
Linezolid Resistant Enterococci in Urinary Tract Infection
Ayekpam Minerva*, Veena Balothia, Rajni Sharma, S.K. Singh,
Department of Microbiology, SMS Medical College, Jaipur, 302004, Rajasthan, India.
* Presenting author: jeenerva@gmail.com
Background
Enterococci are one of the most common isolates in urinary tract infections. It shows intrinsic as well as acquired resistance to a wide range of antibiotics. With the ascending trend of Vancomycin-resistant Enterococci in nosocomial infections, the use of Linezolid has proportionately increased because of its high oral bioavailability and good clinical cure rate. However, cases of Linezolid resistance have also come up in certain strains of Enterococcus species which can be attributed to nosocomial transmission and extensive usage. The study aimed to isolate and identify Linezolid-resistant Enterococcus species among urine samples and study the antimicrobial susceptibility pattern of Enterococcus species isolates at a tertiary care center.
Material & Methodology
An observational study was carried out for a period of 4 months from January 2024 to April 2024 at the Department of Microbiology, SMS Medical College, Jaipur. A total of 478 isolates of non-duplicated Enterococcus species from urine samples received at the Bacteriology Laboratory were processed. Isolation and identification were done using standard microbiological protocols. Antimicrobial susceptibility testing was done on Mueller-Hinton agar by the Kirby-Bauer disc diffusion method as per CLSI guidelines.
Results
Out of 802 urine samples showing positive aerobic growth, 478(59.6%) were Enterococcus species. Among these isolates, 48(10.04%) VRE (Vancomycin-Resistant Enterococci) and 8 (1.67%) Linezolid Resistant Enterococci were detected, all of which were inpatients. Among the Enterococcus species isolates, maximum resistance was seen towards Ciprofloxacin(85.3%) followed by Tetracycline(77%), High.Gentamycin(67%),..Ampicillin(58.5%),Fosfomycin(42%), Nitrofurantoin(25%), Teicoplanin(13.3%), Vancomycin(10.04%) and Linezolid(1.67%).
Conclusion
The emergence of Linezolid-resistant Enterococci poses an alarming threat to clinicians as these isolates have limited or no therapeutic options. Such a condition requires a reduction of inadvertent use of Linezolid by frequent monitoring of antimicrobial susceptibility patterns and strict infection control measures to contain the spread of these multidrug-resistant pathogens.
Abstract 021 ASPICON 2024 |August 22 -25 | 2024 |
The Emergence of Carbapenem-Resistant Enterobacteriaceae (CRE) in Southern Haryana: A Hospital-Based Study
Jyoti Sangwan*, Sarita Sherawat, Pratibha Mane
SHKM Govt Medical College, Nalhar, Nuh, Haryana-122107, India.
* Presenting author: jyolathwal1@gmail.com
Background
In the past two decades increasing number of bacteria in the family Enterobacteriaceae have become resistant to multiple antimicrobial classes leading clinicians to turn to agents from the broad-spectrum carbapenem class for the effective treatment of life-threatening infections caused by these organisms. Therefore present study planned to detect the presence, type, and estimate the burden thereof carbapenemase-producing Enterobacteriaceae.
Material & Methodology
An observational cross-sectional study was carried out from December 2022 to November 2023(1 year) in the department of microbiology of SHKM GMC Nalhar in Haryana. 94 consecutive carbapenem nonsusceptible (by Kirby Bauer Disc diffusion test ) Enterobacterales isolated from various clinical samples were included in the study. Demographic details of patients and samples were included. Identification of isolates to the species level was done using conventional methods. Antimicrobial susceptibility testing of all the isolates was done by Kirby Bauer disc diffusion as per CLSI guidelines. All the carbapenem nonsusceptible isolates by Kirby Bauer disc diffusion method were further subjected to carbapenemase detection by Modified carbapenem inactivation method (mCIM) and further to characterize the type of carbapenemase, EDTA carbapenem inactivation method( eCIM).
Results
570 Enterobacterales were isolated during the study period. 16.49% were carbapenem nonsusceptible by the Kirby Bauer disc diffusion method. These were subjected to mCIM in which 9.5% were found to be positive for carbapenemase production (CRE). 70.4% of Enterobacteriaceae were Metallo-beta-lactamase producers whereas 29.6 % were Serine-type beta-lactamase producers. The majority of isolates were from female and younger age groups. Further most common sample yielding CRE was pus.
Conclusion
Given that carbapenems are the last resort drug for GNBs, there is an urgent need for active antibiotic stewardship in hospitals and communities. Our study underlines the worrisome presence of these CREs in the hospital and hence calls for stringent infection control measures to curb the menace.
Abstract 022 ASPICON 2024 |August 22 -25 | 2024 |
Trends in Antimicrobial Susceptibility Pattern of Salmonella Species Isolated from Bacteremia Patients at a Tertiary Care Center in Northern India
Chinmoy Sahu*, Gerlin Verghese, Nidhi Tejan, Sangram Singh Patel, Rungmei S K Marak
Department of Microbiology, SGPGIMS, Lucknow, Uttar Pradesh, 226014, India.
* Presenting author: sahu.chinmoy@gmail.com
Background
Incidence of Multidrug-resistant (MDR) Salmonella enterica serovars has been increasing globally over the past 20 years which in turn has led to limited options of treatment.
Aim: The study was done to assess the antimicrobial susceptibility pattern among Salmonella enterica serovars causing bacteremia in Northern India. In this observational study, blood samples positive for Salmonella enterica serovars.
Methodology
From January 2021 to April 2023 were studied. Species identification was done using MALDI-ToF MS. Serotyping was done using slide agglutination method using Salmonella polyvalent antisera O, monovalent O:1, O:2, O:9, O:12, and Vi for confirmation of different serovars. Antimicrobial susceptibility was interpreted as per the CLSI guidelines.
Results
During the study period, 32 Salmonella enterica serovars were isolated. Salmonella enterica serovar Typhi was the predominant serovar, followed by Salmonella enterica serovar Paratyphi A. All isolates were susceptible to ceftriaxone, chloramphenicol, co-trimoxazole, and cefotaxime. Pefloxacin showed 100% resistance. Resistance to nalidixic acid was found in 81.2% of isolates. Of the isolates resistant to nalidixic acid, 19(73.08%) isolates were resistant to ciprofloxacin also. Of the 32 isolates, 2 of them were MDR Salmonella isolates. Only one patient died due to the infection. The patient was positive for Salmonella enterica serovar Paratyphi B.
Conclusion
This changing susceptibility pattern necessitates continuous surveillance of antibiogram of Salmonella isolates to rationalize the treatment protocols for invasive salmonellosis and prevent the emergence of resistant strains.
Abstract 023 ASPICON 2024 |August 22 -25 | 2024 |
A Questionnaire-based Survey on the Knowledge, Attitude, and Practice of Antimicrobial Stewardship among the Faculties and Resident Doctors of a Teaching Tertiary Care Hospital in Punjab, India
Shalini Mandal*, Shailza Balu , Navjot Kaur , Jasbir Singh
Department of Pharmacology, Govt. Medical College, Patiala, Punjab, 147001, India.
* Presenting author: shalinimandal92@gmail.com
Background
Antimicrobial stewardship is a coordinated program that promotes the appropriate use of antimicrobials thereby improving patient outcomes and decreasing the spread of infections caused by multidrug-resistant organisms. Due to the rise of antimicrobial resistance (AMR), the efficiency of currently used antimicrobial drugs is declining, making it more difficult and expensive to treat illnesses and harder to manage outbreaks. This has emerged as one of the major public health issues globally. A KAP survey is meant to be a representative survey that aims to elicit what is known (knowledge), believed (attitude), and done (practiced) in the context of the topic of interest.
Material & Methodology
The study will be conducted among practitioners (faculty, senior residents, junior residents) of different departments of our hospital after obtaining ethics approval and informed consent. A pre-designed questionnaire will be used after content validation. A validated questionnaire consisting of 30 questions will be shared among potential participants through either online (Google Forms) or offline modes. The respondents will be given one week to respond. In case there is no response one reminder will be given after 7 days. Existing gaps in the knowledge, attitude, and practice will be identified and presented using descriptive statistics.
Results
The result of this survey will help in comprehending the current status of knowledge, attitude, and practice among faculties and resident doctors.
Conclusion
These results will be used to design a tailored educational program for our healthcare setup.
Abstract 024 ASPICON 2024 |August 22 -25 | 2024 |
Comparative Analysis of Standard Treatment Guidelines for Common Infections in India: Identifying Discrepancies and Opportunities for Harmonization
Jasmeen*, Navjot Kaur, Puneet Kaur, Neetu Sharma
Department of Pharmacology, Government Medical College, Patiala, Punjab, 147001, India.
* Presenting author: jas.sangha1993@gmail.com
Background
Antimicrobial resistance (AMR) is a growing global concern. The availability of multiple standard treatment guidelines (STG) can cause ambiguity among prescribing physicians, resulting in either antibiotic underuse or overuse and thus can exacerbate AMR. In the absence of local or institutional antibiogram data, primary care physicians may face challenges in selecting the correct empiric antibiotic regimen, which may lead to potential errors. Thus, this study aims to compare and contrast various STGs and identify discrepancies that may perplex healthcare professionals.
Material & Methodology
A comparative analysis of various STGs of six common infections in India, i.e., UTI, CAP, Enteric Fever, Acute Otitis Media, Pharyngitis, and PID, was conducted. STG from national sources like ICMR (2019,2022), regional treatment guidelines, e.g., PGIMER, Indian Academy of Pediatrics (2022), Lung India, etc. and international guidelines from CDC 2021, Infectious Disease Society of America (IDSA), CMDT 2024 were included. Ethical approval was not required as the data was available in the public domain. The recommended first- and second-line treatment regimens across these guidelines were compared and any discrepancies in the drug selection, dose, and duration of treatment were identified.
Results
Substantial discrepancies exist among national and international STG, including variations in drug selection, with some guidelines designating a particular drug as a first-line treatment, while others classify it as second-line or fail to mention it altogether. Furthermore, additional discrepancies were observed in dosing regimens or treatment duration, with some guidelines providing a range of doses while others specified a single standard dose.
Conclusion
Wide variation exists amongst the studied national and international STG, which may cause confusion in treatment decisions by prescribers and can potentially contribute to AMR. The findings highlight the need for harmonization and streamlining of treatment guidelines to ensure consistency and evidence-based practice in healthcare.
Abstract 025 ASPICON 2024 |August 22 -25 | 2024 |
Prevalence and Antibiotic Susceptibility Patterns of Haemophilus Species Isolated from Lower Respiratory Samples and Blood Samples of Cancer Patients at a Tertiary Care Hospital
Amrutha T.S*, Santhosh Harkal, Pradnya Samant, Gaurav Salunke
Department of Microbiology, TATA Memorial Hospital, HBNI University, Mumbai, 400 094, India.
* Presenting author: amruthasukumaran49@gmail.com
Background
Haemophilus species are pleomorphic, oxidase-positive, fastidious, capsulated gram-negative coccobacilli that cause invasive diseases such as bacteremia and pneumonia. Cancer patients being immunocompromised are more prone to a wide range of infections including Haemophilus. CLSI-approved treatment for H.influenza includes Ampicillin, Carbapenems, Cephalosporins Fluoroquinolones, and Cotrimoxazole. So, determining their susceptibility pattern is also essential in understanding the antibiotic trend.
Methodology
One-year retrospective analysis of lower respiratory and blood samples of cancer patients was performed in the microbiology department at Tata Memorial Hospital, Mumbai. All samples were processed according to standard microbiological procedures. Haemophilus species identified on VITEK and confirmed with factors V and X were included in the study. Antibiotic susceptibility testing was performed using the Kirby-Bauer disc diffusion method. Biotype determination was done using biochemical reactions.
Results
Haemophilus spp. were isolated mainly from respiratory samples (94.5%) whereas 5.4% were isolated from blood (bacteremia). The majority of the cases were males (64.5%), and 39% were in the age group 50-65 years. The prevalence of Haemophilus species isolated from lower respiratory samples and blood samples was 9.2 %. The distribution of H. influenzae was 81.81%, H. parainfluenza (13.6%), and others (4.5%). In H. influenzae, the biotype III was isolated most frequently (67.2%). All isolates were sensitive to Carbapenems and Cephalosporins, followed by Fluoroquinolones (87.7%), Ampicillin (74.6%), and Cotrimoxazole (30%).
Conclusion
Haemophilus spp. Cause significant respiratory tract infections in cancer patients. H.influenzae tends to be the most common species isolated in biotype III and was found to be the predominant one in our population. Isolates were sensitive to carbapenems and cephalosporins.
Abstract 026 ASPICON 2024 |August 22 -25 | 2024 |
Identification of Novel Inhibitors Against Multi-Drug Resistant Uropathogenic Escherichia coli Using Virtual Screening and Molecular Dynamics Simulation Study
Harpreet Kaur*, Naveen Chaudhary, Vinay Modgil, Balvinder Mohan, Neelam Taneja
Department of Medical Microbiology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India.
* Presenting author: sandhu.preet205@gmail.com
Background
Escherichia coli (E. coli) is a gram-negative bacterial pathogen that poses a significant clinical and epidemiologic challenge. The selection pressure brought by the insufficient use of antibiotics has resulted in the emergence of multi-drug-resistant E. coli in the past ten years.
Material & Methodology
Computational and bioinformatics methods for screening inhibitors have significantly contributed to discovering novel antibacterial agents. One possible target for novel anti-virulence drugs is motility. Motility inhibitors are generally effective at concentrations lower than those required for the antibacterial properties of traditional antibiotics, and they are likely to exert less selective pressure than current medicines. Motility may be essential for bacteria to survive, find nutrients, and escape unfavorable environments and biofilm formation. The FliN is a protein forming the bulk of the C ring of the flagella and is present in multiple copies (more than 100) in bacteria. Its absence in mammals makes it an attractive drug target for drug discovery. Two-thousand seven hundred seventy-eight natural compounds from the ZINC library were screened against FliN (PDB ID: 4YXB) using PyRx AutoDock Vina, and the top compounds were selected for secondary screening after sorting the results based on their binding energy.
Results
Based on interactional analysis, binding energy (− 7.78 kcal/mol), and inhibition constant (1.98μM), ZINC000000619481 was the best inhibitor. This compound binds exactly as per the defined active site residues of the receptor protein. Also, molecular dynamics was performed. The eigenvalue of the selected complex was 1.241657e−05. There were no ADME properties outside of the specified range for the identified hit; it fitted exactly to the binding site of the FliN receptor well and was found to be stable in MD simulation studies.
Conclusion
Further in vitro and in vivo studies are needed to confirm its antibacterial activity and use as a potential antimicrobial drug against urinary tract infections caused by E. coli.
Abstract 027 ASPICON 2024 |August 22 -25 | 2024 |
Comparative In Vitro Efficacy of Generic and Branded Levofloxacin, Ceftriaxone and Meropenem Injections
Guru Mehar Sharma*, Shashi Marko, Lily Dubey, PVR Narendra Babu, Prashant Parmar
Department of Pharmacology, Government Bundelkhand Medical College, Sagar, Madhya Pradesh, 470001, India.
* Presenting author: gurumeharsharma1993@gmail.com
Background
The broad acceptance of generic drugs encounters challenges related to their quality, effectiveness, and regulatory scrutiny, leading to significant bias against their substitution. Evaluating the therapeutic effectiveness of both branded and generic antibiotics becomes essential as antibiotic resistance grows. The WHO estimates that a considerable portion of circulating antibiotics, particularly in developing nations, is sub-standard. These substandard antibiotics can result in treatment failure and prolonged illness, significantly contributing to the global antimicrobial resistance (AMR) issue.
Aim & Objective: To assess and compare the In Vitro efficacy of Generic and Branded Injections of Levofloxacin, Ceftriaxone, and Meropenem
Methodology
One generic and one branded formulation of Levofloxacin, Ceftriaxone, and Meropenem were selected for microbiological analysis.Standard(ATCC) bacterial strains of Staphylococcus aureus and Escherichia Coli were used. Standard blank sterile disks were impregnated with 25μl of the Generic and Branded formulations of Levofloxacin, Ceftriaxone, and Meropenem after serial dilutions, achieving a final concentration equivalent to commercially available discs. The antimicrobial activity of the formulations was evaluated using the Kirby Bauer disk diffusion method on Mueller Hinton Agar plates, and zones of inhibition were measured using an Antibiotic zone scale as per CLSI guidelines. Statistical analysis was done.
Results
The mean value of the Zone of inhibition for Generic for Genericfor Generior Generic and Branded formulations of all 3 Antibiotics in both bacterial strains was in the Standard range as per CLSI guidelines.
Conclusion
The study concludes that generic formulations of Levofloxacin, Ceftriaxone, and Meropenem are as effective as their branded counterparts In Vitro. These findings support the use of generic antibiotics as cost-effective alternatives to branded formulations, without compromising therapeutic efficacy. The above study will be further supported with a larger group of samples and variable parameters.
Abstract 028 ASPICON 2024 |August 22 -25 | 2024 |
Myocarditis – A Punch From Gut ”– A Complicated Enteric Fever Case Report
Marapalli Sindhoora*, Manisha Subarao Mane, Syeda Saba Hashmiya, D. Shireesha
Department of Microbiology, ESIC Medical College and Hospital, Sanathnagar, Hyderabad, Telangana 500038
* Presenting author: marapallisindhoora9999@gmail.com
Background
Enteric fever is a common infectious disease occurring worldwide, especially in developing countries. The mortality of enteric fever used to be 10-20% in the pre-antibiotic era. The fatality has significantly decreased to < 1% in the endemic areas with antibiotic treatment. Enteric fever can have diverse extra-intestinal complications including encephalitis, Guillain-Barré syndrome, endocarditis, osteomyelitis, renal abscess, and splenic abscesses. Myocarditis is a rare complication of enteric fever accounting for about 1-5% of affected cases.
Summary of Case
A case 13-year-old girl, presented to pediatric OPD with complaints of fever associated with chills, haematuria, pain abdomen, vomiting, and bi-frontal headache for 4 days with the rest of the vitals being stable. CBP, CUE, Blood culture, Urine culture, CRP, LFT, RFT dengue serology, and Widal were sent. USG abdomen was done which showed no abnormal findings. Urine culture did not show any growth. CRP was found to be in the normal range and Serology for dengue was negative.
Important Findings
Blood culture was flagged positive after 2 days, which was identified to be Salmonella Typhi. 2D Echo and ECG were taken on the background of chest pain which showed LV dysfunction and signs of myocarditis respectively. Based on these, the diagnosis was made as complicated enteric fever for which she received IVIG – 1 dose and Ceftriaxone for 14 days. She recovered fully with reversed 2D echo and ECG changes.
Conclusion
In developing countries like India, rare complications of enteric fever like myocarditis which can occur even in immune-competent cases, pose a diagnostic challenge for paediatricians and can be fatal if not treated properly and timely. Hence ECG and Echocardiography should be part of the regular assessment of enteric fever. These patients should also be under close follow-up till ventricular function is fully recovered.
Abstract 029 ASPICON 2024 |August 22 -25 | 2024 |
Infectious Diseases and the Status of Women in India with a Specific Emphasis on the Caste Aspect
Hemangi Kadlak1*, Dr. Raj Kishore Sahu2
1- Dr Ambedkar Chair, Symbiosis International (Deemed University), Pune – 411 004, Maharashtra, India.
2- International Institute Of Health Management Research – IIHMR, Delhi 110075, India.
* Presenting author: hemangi.kadlak@gmail.com
Background
Biological differences, social determinants, and cultural norms contribute to increased susceptibility and vulnerability to infections among women. Women are more prone to reproductive tract infections and urinary tract infections, fungal infections, and sexually transmitted infections (STIs/RTIs) such as HPV, syphilis, gonorrhea, herpes, and Chlamydia due to biological and behavioural factors. In the patriarchal structure of Indian society, where women often hold subordinate positions, their health is frequently overlooked or deprioritized. This neglect is further compounded by various socio-cultural, educational, economic, and geographical factors that negatively influence women’s health. Indian women are disproportionately affected by a range of infectious diseases, facing a higher likelihood of infection and more severe disease outcomes than men. Due to cultural and economic constraints, underprivileged women face a higher risk of HIV/AIDS infection. Alarmingly, 24% of Indian women are undernourished, while 54% suffer from anemia.
Methods
In-depth interviews of 54 women were recorded using stratified random sampling from different castes (SC, ST, OBC, and general). Women from rural and urban areas with varying education levels and socioeconomic status were included. Secondary data analysis of existing literature and reports were made. Informed consent and Confidentiality and anonymity with Ethical approval from the Institutional Review Board were taken.
Results
Throughout their lives, women are at continuous risk of contracting infectious diseases. Dalit women belonging to lower castes endure the compounded disadvantages of caste and gender discrimination, leading to a life expectancy that is, on average, 15 years shorter than that of upper-caste women. The root causes include poor nutrition, strenuous labor, and inadequate healthcare access. Lower caste women’s access to healthcare is severely restricted, heightening their susceptibility to infectious diseases. WHO reports indicate a higher prevalence of maternal mortality, anemia, and other health issues among lower caste women, exacerbated by poor healthcare access, sanitation, and nutrition. Moreover, social and cultural practices like child marriage and restricted mobility further elevate their disease risk. Addressing the health inequities faced by lower caste women necessitates a comprehensive strategy, including policy reforms, education, and community initiatives. The National Family Health Survey shows a marked disparity in life expectancy between general and lower castes (SC/ST), with a significant risk of HIV-AIDS and prevalent skin conditions among Dalits.
Conclusion
Key to improving women’s health status in India are education, awareness of personal health, economic independence, and autonomy in health-related decisions, particularly reproductive health. We emphasize the need for gender-sensitive public health strategies, improved access to healthcare, and increased research to address the unique needs of women in preventing, diagnosing, and treating infectious diseases. These are crucial measures for enhancing the overall health and wellness of Indian women.
Abstract 030 ASPICON 2024 |August 22 -25 | 2024 |
Analysis of Changing Trends of Antimicrobial Resistance in Enterobacterales Isolates to Commonly Used β-Lactam Antibiotics in a Tertiary Care Hospital: Sub-Himalayan Region
Sharma Manvi*, Kashyap Saleena, Sood Anuradha, Kaur Isampreet, Chaudhary Anuradha
Department of Microbiology, Dr. Rajender Prasad Government Medical College, Kangra at Tanda (H.P.), India.
* Presenting author: smanvi2408@gmail.com
Background
Multidrug-resistance in gram negative bacteria is a global threat, requiring urgent attention. Third-generation cephalosporin-resistant and other broad spectrum β-lactam antibioticresistant Enterobacterales are emerging worldwide and are classified as high-priority pathogens by WHO. Carbapenem-resistant Enterobacterales were uncommon in the past and served as treatment options for these resistant organisms, but the trend is shifting in recent years.
Methods
Study includes retrospective analysis of resistance trend to commonly used parenteral βlactam drugs in Enterobacteriaceae isolates obtained from culture positive clinical samples, between Jan 2022- May 2024 in Department of Microbiology, DRPGMC Tanda.
Results
Total of 8,185 Enterobacterales isolates were obtained from 2022 to 2024. In 2022, a total of 3262 of Enterobacterales were obtained, followed by 3602 in 2023 and 1321 in 2024 (till date). Ceftriaxone showed steadily increasing resistance rates of 60.94% in 2022, 63.32% in 2023 and 65.44% in 2024. Piperacillin-tazobactam showed a drastic increase in rate of resistance from 24.81% in 2022 to 64.50% in 2023 and 72.34% in 2024. Meropenem showed steady resistance rates of 17.29% in 2022, 16.14% in 2023 and 13.85% in 2024.
Conclusion
There is an increase in overall resistance rates during the study period. This could be due to over-the-counter use of broad-spectrum antibiotics, unnecessary antibiotic use, poor adherence to hospital antibiograms by clinicians, poor implementation of HIC and AMSP.
Abstract 031 ASPICON 2024 |August 22 -25 | 2024 |
Trends in Antimicrobial Resistance Patterns Among Gram Negative Non-fermenters in Intensive Care Units of a Tertiary Care Hospital in Eastern India.
Subhra Snigdha Panda1*, Rajesh Kumar Dash1, Nipa Singh1 , Ipsa Mohapatra2, Dipti Pattanaik1, Kalpana Mund1, Preety Mishra1, Soumya Nayak1
1- Department of Microbiology, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, Odisha
2- Department of Community Medicine, KIMS, Odisha
* Presenting author:– subhra.panda@kims.ac.in
Background
Antimicrobial resistance (AMR) is increasing at an alarming rate among Gram negative bacteria (GNB) in intensive care units in recent years and has become a matter of concern around the world.1 Limited availability of evidence-based data and empirical antibiotics, non-fermenting Gram-negative bacilli (NF-GNB) have emerged as noteworthy pathogens in health care setting.2 This study aimed to find out the prevalence of different non fermenter GNB in ICUs and to analyse the trend of antimicrobial resistance of the isolates over a period of 5 years.
Materials & Methods
It is a cross-sectional retrospective study from January 2019 to December 2023 including 993 isolates identified by VITEK 2 from clinical samples of various ICUs in KIMS hospital, Odisha. Data collected was entered into Microsoft Excel spreadsheet, analysed using Epi Info software, presented using descriptive statistics.MH-chi-square was used as a test of significance with a p-value of 0.05 considered statistically significant.
Results
Over a 5 year period the most commonly isolated non fermenter GNB was Acinetobacter spp. (44.6%) followed by Pseudomonas spp. (29.7%) and Burkholderia spp. (13.7%) and other non-fermenter GNB. With advancing age of the patients, a statistically significant increasing trend in presentation of GNB seen in Acinetobacter spp. (p=0.042) followed by
Burkholderia spp. (p=0.048). Decreasing trend of resistance to antibiotics in Acinetobacter spp. were seen for carbapenems (88 % to 81.5%) and ciprofloxacin (86% to 79.6%). Increasing trend of resistance seen for piperacillin/tazobactam (8.8 % to 85.2%) and amikacin (55.6% to 72.2%). In Pseudomonas spp. aztreonam (74.3% to 54.2%) and ceftriaxone (2.9% to 0) showed decreasing trend of resistance.
Conclusion
Acinetobacter spp. is the most common isolated bacteria showing increased sensitivity to carbapenems and Pseudomonas spp. showed increased sensitivity to aztreonam. The trend of antimicrobial resistance highlights for thorough follow up of antibiograms in hospitals and their judicious use by implementation of antimicrobial stewardship.
Abstract 032 ASPICON 2024 |August 22 -25 | 2024 |
Integrating Aerobic and Anaerobic Cultures in Wound Bio-Burden for Surgical Decision Support
Tanvi Vashist1*, Divya Nair1, Nitika Rana1,Vikas Sharma1, Cherring Tandup2, Pallab Ray1, Amit Arora1, Archana Angrup1
1- Department of Medical Microbiology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
2- Department of General Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India
* Presenting author:-tanvipgi@gmail.com
Background
Necrotising soft tissue infections (NSTIs) are rare but severe conditions characterised by rapid necrosis extending into deep fascia. Diagnosis is challenging and delays in treatment can be fatal. Microbiological cultures are essential to identify the causative organisms and understand the infection.
Methods
This study investigated the wound bioburden in 169 ’tissue biopsies from patients with NSTIs using both aerobic and anaerobic cultures. Tissue samples were cultured on blood agar and MacConkey agar plates, incubated under both aerobic and anaerobic conditions, and colonies were identified using MALDI-TOF MS.
Results
Results showed a wide range of bacterial counts, with heavy or overburdened plates reaching 1017 CFU/ml/g, while positive necrotic tissue had a minimum count of 109 CFU/ml/g. Most cases required amputation due to the severity of the infection. A semi-quantitative ranking system (sterile, scanty, mild, heavy, overburdened) based on aerobic blood plates was developed to aid in the rapid assessment of active infection at the point of care, facilitating surgical decision-making.
Conclusion
Integrating aerobic and anaerobic cultures, along with standardized quantitative and semiquantitative assessments, provides a comprehensive understanding of wound bio-burden in NSTI biopsies. This point-of-care knowledge enables timely and informed decisions regarding surgical intervention in cases of active infection.
Abstract 033 ASPICON 2024 |August 22 -25 | 2024 |
Unravelling the Microbiological Silhouette Causing Orthopaedic Infections in a Tertiary Care Centre
Pragyan Swagatika Panda*, Arpita Panda
Department of Microbiology, VMMC and Safdarjung Hospital, New Delhi-29, India
* Presenting author:— pragyanpanda2006@gmail.com
Background
Orthopaedic infection of the bone, joint and associated structures are commonly caused by bacteria, which is acquired either by endogenous or exogenous routes (surgical site, trauma, and implant related infections), posing a global challenge with alarming consequences in resource constrained settings leading to increased medical cost, drug resistance and difficult to manage infections resulting in significant mortality. This study aimed to determine the bacteriological profiles and antimicrobial susceptibility patterns associated with orthopaedic infections.
Methods
An institution-based retrospective study was conducted from Jan 2023 to April 2024 at VMMC and Safdarjung Hospital, New Delhi. About 2467 patients with clinically suspected orthopaedic infections were enrolled. Aseptically collected Wound swabs or pus aspirates were processed aerobically for culture and sensitivity and antibiotic sensitivity testing as per standard microbiological techniques and CLSI 2023. SPSS version 25 was used for analysis.
Results
Most patients were 18-30 years old (34.5%), with a male preponderance (77.4%). The infection was more in winter season (35.6%). Pathogenic bacteria were grown in 54.3% of samples. Staphylococcus aureus (22.5%) and Klebsiella pneumoniae(7.1%) were the most common organisms. Gram positives were mostly resistant to Penicillin, Ciprofloxacin, and Erythromycin, while Gram negatives were mostly resistant to Amoxicillin-clavulanic acid, Cefepime, Cefotaxime, Ciprofloxacin, Piperacillin- tazobactam and Aminoglycosides.
Conclusion
The most isolated bacteria were S. aureus and Klebsiella spp. To mitigate the problem, aseptic surgical practice, conventional wound management, appropriate infection control practices and constant observation of antimicrobial resistant patterns, should be followed.
Abstract 034 ASPICON 2024 |August 22 -25 | 2024 |
Patterns of Antibiotic Prescription in Outpatients at a Public Health Care Facility in a Northern State of India
Anu Nosran1* , Ritika Kondel Bhandari1 , Anil Kumar2 , Sundeep Sahay3,4 , Arunima Sehgal Mukherjee3,4 , Neelam Taneja5 , Nusrat Shafiq1*
1-Department of Pharmacology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India.
2-Department of Medical Microbiology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India.
3-Department of Informatics, University of Oslo (UIO), Oslo, Norway.
4-Society of Health Information Systems Programmes, New Delhi, India.
5-Civil Hospital, Baddi, Himachal Pradesh, India
* Presenting author: anunosran@gmail.com
Objectives
Conducting Outpatient survey (OPS) is especially challenging in the absence of electronic medical records, lack of dedicated resources and a high patient load in resource poor settings. The study aimed to analyze the patterns of antimicrobial prescriptions among patients visiting outpatient departments of a secondary care facility in an industrial town in northern India. This survey was conducted to provide background data for planning and strengthening the antimicrobial stewardship program (AMSP) in a public health care facility in Baddi, Himachal Pradesh.
Methods
A prospective, single-center outpatient survey (OPS) on antimicrobial prescriptions was carried out at Civil Hospital, Baddi, Himachal Pradesh, India. Information on patient demographics, reasons for antimicrobial use, and details of each prescribed antimicrobial, including supportive investigation reports, was collected using predesigned forms. The IEC approval was taken from Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh (IEC No. IEC-10/2022-2575).
Results
From September 2023 to June 2024, a total of 2098 patients were screened for potential eligibility visiting the outpatient facility at Civil Hospital, Baddi. 1400 (66.73%) were prescribed antibiotic(s). The commonest indication for which antibiotic was prescribed was Urinary tract infections (UTI) (24.2%). Majority of prescriptions included single antibiotic (85.7%) and third generation oral Cephalosporin, Cefixime accounted for 42.2% of these prescriptions. Though the majority of prescriptions were oral, 2.6% patients received injectables. Majority of prescriptions were from the ‘Watch’ category of antibiotics. Importantly, the culture facility at the site was used for guiding a treatment in a vast majority, E. Coli was the commonest isolated organism.
Conclusion
The present study gives us a background of prevalent conditions presenting at the setting, profile of organisms and their susceptibility. Secondly, an evidence based policy will be generated for the facility.
Abstract 035 ASPICON 2024 |August 22 -25 | 2024 |
Antibiotic prescription patterns among Admitted Patients in a tertiary Healthcare Facility in India: findings from a Point Prevalence Survey
Vinay Modgil1*, Rashmi Surial1, Oshin Sinha1, Sahil Kumar1, Mallika Nanda1, Arunima Mukherjee1,2, Sundeep Sahay1,2, Sunil Kumar Raina3, Raman Chauhan3
1. Society for Health Information Systems Programmes (HISP India), New Delhi, India
2. Department of Informatics and Centre of Sustainable Healthcare Education (SHE), Faculty of Medicine, University of Oslo, Oslo, Norway
3. Department of Community Medicine, Dr. RP Government Medical College, Kangra at Tanda, Himachal Pradesh
* Presenting author: Vinay.modgil@hispindia.org
Background
In India, data on antibiotic prescription patterns at the patient level is scarce, and intervention measures to optimize antibiotic prescription patterns and reduce antimicrobial resistance are rarely performed. This study aims to determine the antibiotic prescribing pattern in admitted patients in the tertiary care hospital, in North India.
Methods
A Point Prevalence Survey (PPS) on antibiotic prescription patterns according to the World Health Organization (WHO) Methodology for PPS on antibiotic prescription in hospitals, was carried out in tertiary care hospitals. PPS was conducted over 2 weeks across five different wards in this hospital. Eligible inpatients were those who were hospitalized in the ward at 8.00 a.m. on the day of the survey.
Results
In our findings, the overall prevalence of antibiotic usage among inpatients was 62%. Empirical treatment of antibiotic prescriptions was found in 95.2% of the patients. In 10% of patient’s bacterial culture and AST were performed. In most of the patients, an antibiotic course was started before the sample was sent for culture, and cultures were sent on the 2 nd or 3 rd day of admission. The antibiotic ceftriaxone, which belongs to the WHO “watch” category, was the most prescribed antibiotic (49%), followed by azithromycin (16.40%) and metronidazole (16%), both belonging to the WHO “access” group of antibiotics. Overall, parenteral routes of antibiotic administration were common in 84% of patients, whereas oral drugs were given only in 19% of the patients. We observed that 30% of patients received more than one antibiotic and broad-spectrum antibiotics were prescribed in more than 50% of cases. Antimicrobial prescriptions for both medical and surgical prophylaxis were 23% and 12% respectively.
Conclusion
In conclusion, the findings suggest the need for strengthening diagnostic and antimicrobial stewardship programs given the high proportion of antibiotic use, underutilization of bacterial culture, and complete reliance on empirical antibiotic treatment. Furthermore, this study has identified areas for quality improvement, including education programs focusing on prescription practice in admitted patients and the urgent need for antimicrobial stewardship policy in hospital settings.
Abstract 036 ASPICON 2024 |August 22 -25 | 2024 |
Evaluating the consumption pattern of antibiotics in the In-patient clinical department of a tertiary care hospital by using WHO AWaRe and DDD/100 bed-days
Vikash Kumar Bhati*, Shashi Marko, Lily Dubey
Department of Pharmacology, Government Bundelkhand Medical College, Sagar, Madhya Pradesh, India.
* Presenting author:— vikaskumarbhati12@gmail.com
Background
Antibiotic resistance is on rise and has become a worldwide problem, because of higher utilization and irrational uses of antibiotics. Consumption patterns of drugs can be classified by WHO AWaRe and measured by ACT/DDD/100 bed-days (Define daily dose) methodology. Surveillance data of antibiotics consumption can be used for developing hospital antibiotic policy as well as stewardship programs.
Methods
Detailed data of antibiotic dispensed to various clinical Inpatient (IPD ) from 01/04/ 2023 to 31/03/ 2024 was collected from Central hospital pharmacy and pattern of use and consumption was calculated in terms of ACT/DDD and AwaRe Classification.
Results
Total 19 antimicrobials were used during the study period. Out of which 6 (Access), 7 (Watch), 1 (Reserve), 5 (Non-recommended) and 13 (E.M.L.), 1 (Non-EML) and 5 (Non-classified). Majority Cephalosporin (54.60%, {Ceftriaxone 31.12 DDD/100 bed-days and Cefotaxime 5.1 DDD/100 bed-days) class of drug were most commonly used followed by imidazole derivatives (16.97%, 8.2 1 DDD/100 bed-days) and lastly penicillin including beta-lactamase inhibitor (6.11%, 2.55).
Conclusion
As the data shows in comparison to antibiotics of the Access category, antibiotics of the Watch group were used more frequently and should pay attention toward the non recommended category because consumption of this class is also a considerable amount. 3-4 antibiotics are used more than others that will lead to resistance. Institutions must go for an antibiotic policy and stewardship program that will help to procure and dispense the antibiotics as per requirements.
Abstract 037 ASPICON 2024 |August 22 -25 | 2024 |
An Evaluation of Antibiotic Prescription Pattern and Drug RationalityAnalysis Among Outpatients at public health setting, India
Vinay Modgil1*, Amandeep Gondara 1, Rashmi Surial1, Harpreet Singh 2, Vivek Karol3, Nusrat Shafiq* 4, Neelam Taneja* 1
1-Department of Medical Microbiology, Postgraduate Institute of Medical EducationandResearch, Chandigarh. India.
2. Department of Medicine, Postgraduate Institute of Medical Education and Research, Chandigarh. India.
3 Civil Hospital Kangra, Himachal Pradesh, India
4. Department of Pharmacology, Postgraduate Institute of Medical Education and Research, Chandigarh. India.
* Presenting author:– vnmodgil@gmail.com
Background
Antimicrobial resistance (AMR) poses a significant threat to global public health, increasingly prevalent due to inappropriate antibiotic prescribing patterns. Rational prescribing is essential to combat AMR, as rational analysis can identify irrational practices and build physician consensus. This study evaluates antibiotic prescription patterns and assesses the rationality of drug use among outpatients in a public health setting in India.
Methods
A cross-sectional study was conducted at a 30-bed public community health centre serving a population of 12,900, including urban and rural residents, between August 2021andAugust 2022. Data were collected from 1,219 outpatient antibiotic prescription slips, randomly selected, and analyzed for drug type, dosage, duration, and adherence to clinical guidelines. For rationality assessment, each prescription was analyzed by a team of ID specialists (HS) and infectious disease clinical pharmacologists (NS) based on standard principles of rational prescriptions of antimicrobials. When required, NCDC treatment guidelines for infections, guidelines for the management of infections by the PostgraduateInstitute of Medical Education and Research, and standard reference guidance documents were referred. Data was analyzed to evaluate demographics, the most prescribed antibiotics their class and AWaRe category, diagnoses among these patients, drug rationality, and the drugs from the Essential Drug List (EDL).
Results
A total of 1,219 antibiotic prescription slips were analyzed. Among these, 45.9%were for males and 54% for females, with most patients (30.9%) being aged 20-40 years. Oral infections (21.4%) were the most common diagnosis followed by Skin and soft tissue infection (20%). The most frequently prescribed antibiotic was amoxyclav (27.2%), followed by metronidazole (13.4%) and azithromycin (10.3%). According to the WHOAWaReclassification, 49.7% of the prescribed antibiotics were in the “Access” group, while 27.3% were in the “Watch” group. No antibiotics were prescribed from the “Reserve” group. Regarding rationality, 57% of prescriptions for urinary tract infections were rational, whereas only 29% of respiratory tract infection (RTI) prescriptions were rational. Diarrhea cases showed the highest rate of irrational antibiotic use (95%) followed by RTI (71%).
Conclusion
The study highlights significant issues in antibiotic prescription practices, with a considerable proportion not adhering to recommended guidelines. These findings underscore the necessity for optimized antibiotic prescribing practices to combat AMRinoutpatient settings in India. Implementing targeted education programs for health care providers, enhancing prescription monitoring systems, and adhering to evidence-based guidelines are critical steps to promote rational antibiotic use and improve public health outcomes.
Abstract 038 ASPICON 2024 |August 22 -25 | 2024 |
Descriptive Analysis of Antimicrobial Resistance Patterns in WHO-Critical Priority Pathogens from Clinical Samples in ICU at a Tertiary Care Hospital, India
Isampreet Kaur1*, Anuradha Sood1, Anuradha Chaudhary1, Vinay Modgil 2
1. Department of Microbiology, Dr. RP Government Medical College, Kangra at Tanda, Himachal Pradesh, India.
2. Society for Health Information Systems Programmes (HISP India), New Delhi, India
* Presenting author:– isampreet@gmail.com
Background
Antimicrobial resistance (AMR) is a serious concern to world health, especially in intensive care units (ICUs) where patients are more susceptible to infections. The World Health Organization (WHO) has identified certain pathogens as a critical priority due to their high resistance rates and limited treatment options. It includes A. baumannii (carbapenem-resistant), P. aeruginosa (carbapenem-resistant), and Enterobacteriaceae (carbapenem-resistant and third-generation cephalosporins resistant). This study aims to provide a comprehensive analysis of AMR patterns in WHO-critical priority pathogens isolated from clinical samples in the ICU of a tertiary care hospital in India.
Methods
Clinical samples were received from the ICU between January 2021 to December 2023. These clinical samples were processed by using conventional culture methods in the microbiology laboratory. Antibiotic susceptibility testing (AST) was performed by using disc diffusion methods as per CLSI guidelines. The pathogens were categorized according to the WHO priority list, and their resistance patterns were analyzed.
Results
A total of 4,339 clinical samples were received from the ICU. From clinical samples, 850 WHO-critical priority pathogens were identified. The most common isolates were A. baumannii 365 (43%) followed by K. pneumoniae 192 (23%), P. aeruginosa 178 (21%), and E. coli 115 (13%). The resistance to carbapenems was observed to be 88% in A. baumannii and 36% in P. aeruginosa. In Enterobacteriaceae, carbapenem resistance was found to be 54%, while resistance to third-generation cephalosporins was 81%.
Conclusion
The antibiotic resistance among critical priority pathogens observed in this study reflects a significant challenge in treating ICU infections in a tertiary care hospital in India. The high rates of resistance necessitate urgent action in implementing robust antibiotic stewardship programs and enhancing infection control practices to mitigate the spread of resistant pathogens. The data generated can aid in developing targeted treatment guidelines and policy decisions to combat AMR effectively.
Abstract 039 ASPICON 2024 |August 22 -25 | 2024 |
Resistance Profile of Candida Isolates in Women with Vulvovaginal Candidiasis Attending Gynecology OPD in a Tertiary Care Hospital
Anisha Yadav*, Ashima Katyal, Deepinder Singh, Prerna Aggarwal, Richa Kansal
Kalpana Chawla Government Medical college, Karnal, India.
* Presenting author:– aannii9@gmail.com
Background
Vulvovaginal Candidiasis (VVC) is a substantially common mucosal infection of the female genital tract caused by a polymorphic opportunistic fungus Candida spp. Over the years, a marked rise in vaginal yeast infections has been observed. Over the counter availability and rampant use of antifungals have contributed massively in development of antifungal resistance, thus have been conducive to increased morbidity among females with VVC.
Methods
197 (HVS) samples were collected from symptomatic females having at least one of the symptoms of itching, vaginal discharge and burning sensation. The samples were processed and subjected to antifungal susceptibility (AFS) by both Kirby Bauer Disc Diffusion(DD) method and by using Octofungi 1 HiMIC plate kit. Three drugs were used for both the methods- fluconazole, voriconazole and caspofungin. The data was analysed statistically and comparison of the resistance pattern by both the methods was done and depicted in the form of a comparative table and graph.
Results
Of 197 samples, 52 were positive for VVC. The species isolated were C. albicans(26), C.parapsilosis (10), C. tropicalis(9), C. krusei(5) and C. glabrata(2). For fluconazole, C. albicans, C. tropicalis showed no resistance by DD method and MIC testing. However, (1/2) of C. glabrata showed resistance by disc diffusion whereas both(2/2) were resistant by MIC. Regarding voriconazole, 3.8% resistance was observed for C. albicans, 50% for C. glabrata, 10% for C. parapsilosis and 11.1% for C. tropicalis by MIC testing. Similarly, for caspofungin, all species were susceptible to DD. Whereas , C. krusei, and C. tropicalis showed no resistance by MIC but C. albicans (3.8%), 50% C. glabrata and 10% C. parapsilosis showed resistance by MIC testing.
Conclusion
Testing by MIC method is a better method for antifungal susceptibility testing, as described by CLSI. Since resistance in Candida isolates is on a rise, it is important to incorporate routine AFS testing which would improve patient outcomes and ultimately reduce morbidity and mortality.
Abstract 040 ASPICON 2024 |August 22 -25 | 2024 |
Prevalence and Antimicrobial Susceptibility Profile of Multidrug Resistant S. maltophilia Causing Infections in a Tertiary Healthcare Setting in North India
Tanya Arora*, Barnali Kakati, Nupur Koul
Himalayan Institute of Medical Sciences, SRHU, Jollygrant, Dehradun
* Presenting author:– tanya1108arora@gmail.com
Background
Stenotrophomonas maltophilia is an emerging opportunistic pathogen in healthcare settings. It is notoriously resistant to many antimicrobials intrinsically and has shown acquired resistance increasingly to many antimicrobials due to multiple drug resistant mechanisms, making therapeutic management of critical cases difficult. This study aimed to determine the prevalence and antimicrobial susceptibility profile of S. maltophilia causing infections at a tertiary hospital setting.
Methods
This observational study was conducted for a one-year duration from 1st May 2023 to 31st May 2024 in the department of microbiology after taking ethical approval from the institute’s ethical committee. All clinical samples received were subjected to aerobic culture at 37°C. Identification and susceptibility testing was performed using VITEK 2 COMPACT automated systems. Antimicrobial susceptibility profile was interpreted in accordance with CLSI breakpoints.
Results
Out of 1870 non lactose fermenters isolated after aerobic culture from various clinical specimens, 66 (3.52%) were identified as S. maltophilia. The isolates were predominantly recovered from 41-60 (34.84%) age group. A male predominance of 1.5:1 was seen. The isolates were identified as multi drug resistance organisms (MDROs) and were found sensitive to minocycline (80.73%), levofloxacin (71.21%), cotrimoxazole (63.36%), ticarcillin and clavulanic acid (62.12%) and chromaphenicol (59%). Resistance was seen predominantly for tetracycline (100%) and ceftazidime (61%).
Conclusion
Although a low prevalence of S. maltophilia was reported at our setup, the antimicrobial susceptibility profile determined would be useful in selection of appropriate antimicrobials to manage infections caused considering the paucity of data on the same.
Abstract 041 ASPICON 2024 |August 22 -25 | 2024 |
Isolation of Cedecea lapagei in a Case of Hemothorax: A Rare Emerging XDR Organism
Bhawna Sharma*
* Presenting author: 34bhawnasharma@gmail.com
Background
Cedecea is a gram negative bacteria belonging to the Enterobacteriaceae family with six known species of Cedecea. Among them three of these species are said to be human pathogens: Cedecea davisae, Cedecea lapagei and Cedecea neteri. It was first described in 2006 as a potential pathogen in a peritoneal fluid of a 55 years old man having peritonitis. Cedecea lapagei was further isolated in pneumonia, bacteremia, soft tissue infection, peritonitis, sepsis, hemoptysis and urosepsis patients. Till now, only thirteen cases of Cedecea lapagei have been described in the literature and none of them was extensively drug resistant.hilia causing infections at a tertiary hospital setting.
Case Summary
A 60 year old female patient of a road traffic accident was brought to the emergency department at AIIMS Bathinda with a history of difficulty in breathing for 1 day. She was diagnosed with hemothorax & subsequently an intercostal drain tube was placed. On day 7th, the patient developed a fever, so ICD content were sent for microbiological bacterial culture and
susceptibility. Growth of Cedecea lapagei was obtained on the culture which showed resistance to piperacillin tazobactam, cefuroxime, ceftazidime, ceftriaxone, cefepime, ertapenem, imipenem, meropenem, doxycycline, tetracycline, amikacin, gentamicin, ciprofloxacin, cotrimoxazole and intermediate susceptible to cefaperazone- sulbactam and susceptible to minocycline only. Repeat sample was taken to exclude the contamination and for confirmation of suspected bacteria. Same organism with a similar susceptibility pattern was obtained on repeated culture. Patient was put on minocycline and after 3 days a sample was sent which was sterile after 48 hours of incubation. Patient became afebrile and the ICD tube was removed. Patient was discharged under stable conditions.
Conclusion
We report a rare case of hemothorax having infection of Cedecea lapagei which was muti-drug resistant. Earlier it was rarely described in the literature to be extensively drug resistant. Hence, early identification of this bacteria and correct antibiotic treatment is important for good outcome.
Abstract 042 ASPICON 2024 |August 22 -25 | 2024 |
Surgical Site Infection in Pediatric Population: Incidence, Etiology and Risk Factors
Prerna Khurana1*, Shariqa Qureshi1, Mamta Senger2
1- Department of Clinical Microbiology and Infectious Diseases, Chacha Nehru Bal Chikitsalaya, Delhi, India.
2- Department of Pediatric Surgery, Chacha Nehru Bal Chikitsalaya, Delhi, India.
* Presenting author:– prernakhurana@gmail.com
Background
Surgical site infection (SSI) is one of the most common healthcare-associated infections (HAIs). However, there is a lack of data available about SSI in children, especially from low-income and middle-income countries. In children, SSI has important social and economic consequences, leading to loss of school days and lost working days by parents. The burden of SSI in terms of healthcare costs and the requirements for antibiotic therapy have important consequences for antibiotic resistance and health system capacity.
Methodology
A retrospective study was conducted over a period of 5 years from January 2019 to December 2023 to study the incidence, etiology and risk factors of SSI in children less than 12 years of age undergoing gastrointestinal, urological and orthopaedic surgery in a government paediatric tertiary care centre.
Result
Over a period of 5 years, samples from 12628 surgeries were conducted, out of which, 365 patients developed SSI, SSI rate being 2.89 SSI per 100 operative procedures. Out of these 365 patients. 55.9% of patients were males and 44.1% were female patients. 14.8% of these patients were neonates. In 10.4% of the patients, infection was present at the time of surgery (PATOS). The most common causative agent of SSI was found to be E.coli (49%), followed by polymicrobial growth (15.9%), and Acinetobacter baumannii (7.7%). The most common risk factors associated were low birth weight, malnutrition, lack of traffic control in OT, patients not taking pre operative showers, longer duration of surgeries, anastomosis leak, inadequate staffing for post op care in ward, and contamination of incision post op.
Conclusion
SSI represents a significant burden of postoperative morbidity in children who receive surgery. Focused initiatives and research, aiming to reduce SSIs in children should be a key priority for surgery agendas.
Abstract 043 ASPICON 2024 |August 22 -25 | 2024 |
3-Step Model- An Explorative Novel Approach to Classify Sepsis: A Longitudinal Observational Study
Jaideep Pilania*, Prasan Kumar Panda
Department of Internal Medicine, AIIMS Rishikesh, India.
* Presenting author:– jaideep.pilania1414@gmail.com
Introduction
Sepsis remains a critical healthcare challenge worldwide, demanding prompt identification and treatment to improve patient outcomes. Given the absence of a definitive gold standard diagnostic test, there is an imperative need for adjunct diagnostic tools to aid in early sepsis detection and guide effective treatment strategies. This study introduces a novel 3-step model to identify and classify sepsis, integrating current knowledge and clinical guidelines to enhance diagnostic precision.
Methodology
This longitudinal observational study was conducted at a tertiary care teaching hospital in northern India. Adult patients admitted with suspected sepsis underwent screening using predefined criteria. The 3-step model consisted of Step 1, assessing dysregulated host response using a National Early Warning Score-2 (NEWS-2) score of ≥6; Step 2, evaluating risk factors for infection; and Step 3, confirming infection presence through clinical, supportive, or confirmatory evidence. Patients were categorized into Asepsis, Possible sepsis, Probable sepsis, or Confirmed sepsis at various intervals during hospitalization.
Result
A total of 230 patients were included. Initial categorization on Day 1 showed 13.0% in Asepsis, 35.2% in Possible sepsis, 51.3% in Probable sepsis, and 0.4% in confirmed sepsis. By Day 7, shifts were observed with 49.7% in Asepsis, 9.5% in Possible sepsis, 25.4% in Probable sepsis, and 15.4% in confirmed sepsis. At discharge or death, categories were 60.4% Asepsis, 5.2% Possible sepsis, 21.7% Probable sepsis, and 12.6% Confirmed sepsis. Transitions between categories were noted throughout hospitalisation, demonstrating the dynamic nature of sepsis progression and response to treatment.
Conclusion
The 3-step model effectively stratifies sepsis status over hospitalization, facilitating early identification and classification of septic patients. This approach holds promise for enhancing diagnostic accuracy, guiding clinical decision-making, and optimizing antibiotic stewardship practices. Further validation across diverse patient cohorts and healthcare settings is essential to confirm its utility and generalizability.
Abstract 044 ASPICON 2024 |August 22 -25 | 2024 |
Bacteriological Profile and Antimicrobial Susceptibility Pattern in Blood Culture Specimen in a Tertiary Care Hospital of Uttar Pradesh: Six Years Retrospective Study
Shweta Singhal*, Pragya Shakya, Arti Agarwal, Ankur Goyal
Department of Microbiology, Sarojini Naidu Medical College, Agra, India.
* Presenting author:– singhals10@gmail.com
Background
Globally, bloodstream infections (BSI) are major contributors to morbidity and mortality. Antimicrobial surveillance is crucial for spotting emerging resistance and developing empirical treatment guidelines. The goal of this study is to examine trends in BSI antimicrobial susceptibility from 2018 to 2023 in a tertiary care centre.
Methodology
This was a retrospective study conducted in the department of microbiology, Sarojini Naidu Medical College, Agra. Blood samples for culture were received from various clinical departments which were processed by conventional methods for identification.
Result
4195 samples were tested positive from a total of 11882 samples. Most of the samples that tested positive were from the pediatric age group. Klebsiella species was the most frequent organism to be isolated (45%) amongst the gram-negative organisms followed by E. coli species (30.9%). Other gram-negative bacilli that were isolated included Burkholderia species, Acinetobacter species, Pseudomonas species, and Citrobacter species. While klebsiella species demonstrated a decline in resistance to doxycycline and ceftriaxone sulbactam antibiotics, they demonstrated a significant rise in resistance to imipenem and piperacillin tazobactam antibiotics. However, there was no change in the resistance pattern of cotrimoxazole and ceftriaxone during the years. Antibiotic resistance to amikacin, piperacillin, tazobactam, and cotrimoxazole increased significantly in the E. coli isolate, while antibiotic resistance to levofloxacin, doxycycline, and ceftriaxone decreased in these 6 years’ time. Among the various antibiotic groups, Pseudomonas species exhibited the highest emergence of resistance, with the exception of piperacillin and carbapenem antibiotics.
Conclusion
Rising resistance to last-resort antibiotics such as beta-lactam and carbapenem antibiotics, especially in Gram-negative bacteria, indicates that there is urgent need for exploring new antibiotics such as Fosfomycin, tigecycline and other antibiotics against these carbapenem resistant isolates and stronger antimicrobial stewardship efforts to combat antimicrobial resistance and stop the spread of multidrug resistant bacteria amongst population.
Abstract 045 ASPICON 2024 |August 22 -25 | 2024 |
Analysis of Antibiotic Consumption Patterns, Practices and Trends Based on Procurement Data of Public Health Institutions in the Hilly State of Himachal Pradesh, India. (2018-2022)
Rashi Banta*, Neha Joshi, Subhash Chand
Society for Health Information System Programmes (HISP India)
* Presenting author:– rashi.banta@hispindia.org
Introduction
India, despite being the largest consumer of antibiotics in absolute volume, lacks a formal system for antibiotic use unlike the US and Europe. Consequently, much antibiotic use data remains “invisible.” This paper aims to make antibiotic use data within the public health sector of a northern Indian state “visible”.
Methodology
This study analyzes antibiotic use patterns and trends in five Public Health Facilities in Himachal Pradesh from 2018 to 2022. The analysis employs the Anatomical Therapeutic Chemical (ATC) classification system and uses Defined Daily Dose (DDD) and Drug Intensity Dosage (DID) as metrics.
![]()
Using the formula where:
Yi: The adjusted DDDs in a given year in a certain type of healthcare institution i;
Mi: DDDs used in a given year in a certain type of healthcare institution i;
ni: Number of a certain type of healthcare institution i from where data was collected; PHC, CHC, DH, Tertiary and Super Speciality Hospitals
Ni: The total number of a certain type of healthcare institution i in the Health Statistics Yearbook
Result
This study examines antibiotic procurement in Himachal Pradesh from 2018 to 2022. During this period, total antibiotic consumption initially increased, peaking in 2019, a sharp decline in 2020, due to COVID 19 followed by a steady rise and then a decline in 2022. The most commonly consumed drug classes were Macrolides followed by Fluoroquinolones and Penicillins whereas Cephalosporins & Carbapenems were the least consumed.
Conclusion
This study provides empirical evidence on trends in antibiotic procurement and expenditure from 2018-2022. The introduction of an essential drug list by the state government improved medicine availability at hospital pharmacies. Concurrently, interventions like prescription audits, digitization of procurement and consumption data, and antimicrobial stewardship have arguably contributed to the decrease of antibiotic consumption. However, the patterns of antibiotic use do not provide strong evidence to show rational use of antibiotics.
Abstract 046 ASPICON 2024 |August 22 -25 | 2024 |
Identification of Factors Driving Decision Making in Prescribing Empirical Antibiotics-An Observational, Cross-sectional Pilot Study
Avinash Turankar, Sukant Pandit, Kritika Milind Dongre, Sivasakthi C*
Department of Pharmacology, Government Medical College, Nagpur, India
* Presenting author:– shaksiva1997@gmail.com
Introduction
Antimicrobial Stewardship requires multiple stakeholders who are responsible for patient care. Hence it is prudent to understand the factors which are responsible for decision making for prescribing empirical antibiotic therapy. The pilot study aims to identify the attributes and its levels affect decision making while prescribing empirical antibiotic therapy.
Methodology
An observational, cross-sectional study with study Population of 200 Registered medical practitioners will be done from May 2024 to July 2024 online through Google forms. An e-Informed consent will be taken before attempting the questionnaire in which the purpose of the study will be explained. Demographic profile of the doctor including the place of his practice (urban, rural) and type of practice (private, government) and his/her qualification along with the years of experience will be taken. A total 15 questions will be asked which shall not take more than 10 minutes to answer.
Result
Although data collection is ongoing, preliminary projections suggest that factors such as antibiotic spectrum, adherence to clinical guidelines, and patient-specific characteristics (e.g., age, comorbidities) are likely to emerge as significant drivers in the decision-making process. Cost is anticipated to have a moderate impact.
Conclusion
After completion of data analysis, the study will highlight the factors or attributes affecting the decision for prescribing empirical antibiotics. These insights will help in tailoring solutions for enhanced acceptance and implementation of antimicrobial stewardship by the clinicians. The results will help us conduct a robust and validated discrete choice experiment study.
Abstract 047 ASPICON 2024 |August 22 -25 | 2024 |
Efficacy of Conventional and Molecular Methods in Clinically Suspected Cases of Musculoskeletal Tuberculosis in a Tertiary Care Hospital
Pandey P*, Rai B, Bhatia NJK, Shulania A
Department of Microbiology, ABVIMS &Dr. RML Hospital, New Delhi, India.
* Presenting author:– drpragyap1@gmail.com
Objective
Lab diagnosis of clinically suspected cases of musculoskeletal tuberculosis by ZN staining, MGIT, and CBNAAT.
Material & Methodology
The samples were collected in the Department of Microbiology in association with the Department of Orthopaedics between August 2022 to March 2024. Eighty clinically suspected musculoskeletal tuberculosis patients were included and the samples were processed for ZN staining, CBNAAT, and MGIT.
Result
The mean age of the study population ranged from 1.5 to 69 years with a maximum number of cases aged between 21 and 30 years (23.98%). Knee joints (n=33; 41.3%) followed by spine (n=31; 38.8%) were the most commonly involved sites. In half the cases (n=40; 50%), the specimen was fluid aspirate from the affected site,33 (41.3%) were pus specimens and 7(8.8%) were biopsy specimens. The positivity rate for Ziehl-Neelsen staining and MGIT was 11.3% and 12.5% respectively. A total of 18 (22.5%) cases were confirmed as tuberculosis. ZN stains had the lowest sensitivity, negative predictive value, and accuracy (50%, 87.3%, and 88.8% respectively) followed by MGIT (55.6%, 88.6%, and 90% respectively). However, CBNAAT was not only highly sensitive (94.4%) but also had high negative predictive value (98.4%) and accuracy (98.8%).
Conclusion
The present study showed that CBNAAT is a useful, sensitive and specific molecular diagnostic method compared to MGIT and ZN stain for evaluation of extrapulmonary tuberculosis so the CBNAAT could be recommended as the first line diagnostic method for the detection of tuberculosis in clinically suspected musculoskeletal tuberculosis cases.
Abstract 048 ASPICON 2024 |August 22 -25 | 2024 |
Achromobacter Species: An Underestimated Contributor to Post-operative Infections in Immunocompromised Patients in a Tertiary Care Cancer Center
Anwita Mishra1*,Vijeta Bajpai1, Shashank Tiwari2, Prity Gupta1, Rahul Sarode1, Sujit Bharti1
1- Department of Microbiology, Homi Bhabha Cancer Hospital, Mumbai, India.
2- Department of Microbiology, Mahamana Pandit Madan Mohan Malviya Cancer Centre, Uttar Pradesh, India.
* Presenting author:-anwitajan18@gmail.com
Background
Achromobacter is a genus of non-fermenting Gram-negative bacteria under order Burkholderiales. They are mostly associated with the respiratory tract of patients with cystic fibrosis. They are often isolated from severe healthcare-associated infections in immunocompromised patients.
Case Summary
A total of 8 cases of infections due to Achromobacter spp. were identified in the year 2023 at our centre; 4 cases each of A. denitrificans, and A. xylosoxidans. Most of the patients were males from 40 to 80 years of age. All the patients were diagnosed with advanced stage solid organ cancers and had undergone surgery in the recent past, with the patients belonging to head and neck tumours accounting for the maximum cases. None of the above patients were lost during treatment and follow-up.
Important findings
Heavy growth of A. denitrificans was isolated from chemo port catheter and pus swab from pus/discharge oozing from surgical wounds. Significant growth of A. xylosoxidans was also isolated from urine, bronchoalveolar lavage and pus swab of post-operative admitted patients. The isolates were identified by manual biochemical reactions and the Vitek-2 automated ID and susceptibility testing system. A. xylosoxidans isolates showed high susceptibility to cotrimoxazole, cefoperazone-sulbactam and ceftazidime, and resistance to fluoroquinolones. A. denitrificans isolates showed high susceptibility to piperacillin-tazobactam and resistance to fluoroquinolones. Although the infections were serious, requiring ICU admission for some patients and long-term therapy, all the above patients recovered successfully.
Conclusion
These cases illustrate the important role of this bacterium in serious infections in patients with advanced-stage cancers of solid organ systems. Although infections reported by these bacterial isolates are less frequent, they can be a serious threat to immunocompromised patients. Differences in biochemical reactions and antibiotic susceptibility patterns from other commonly isolated Gram-negative bacteria should be borne in mind for rapid diagnosis and prompt institution of appropriate therapy.
Abstract 049 ASPICON 2024 |August 22 -25 | 2024 |
Mycetoma in North India: A Clinico-epidemiological and Investigative Study- New Patterns of a Neglected Tropical Disease
Nidhi Sharma*, Devraj Dogra, Basira Sultan
Department of Dermatology, GMC Jammu. India.
* Presenting author:-: Needee88@gmail.com
Background
Mycetoma is a chronic, suppurative granulomatous infection affecting skin and subcutaneous tissues and is characterized clinically by a triad of painless soft tissue swelling, underlying sinus tracts, and extrusion of grains. It is endemic in India and other tropical and subtropical countries between latitude 15° S and 30° N all around the globe.
Methodology
This study involved a cross-sectional design in which cases of mycetoma presenting to a tertiary care hospital in north India were included. Clinicoepidemiological parameters including age, gender, occupation, geographical distribution and site of involvement were noted. Diagnostic investigations included microbiological and histopathological analyses of the clinical samples. Radiological studies including X-ray/ultrasound and MRI were done to evaluate the extent of tissue involvement.
Result
A total of seven cases were studied. Female outnumbered males (71%) and age of the patients varied from 13-71 years. Site of involvement was right foot in 57.1% cases and left foot in 42.8% cases. 85% of the patients had occupational exposure in the form of working in fields. There was a history of passage of granules in 4 patients, however pale white granules were retrieved only in 2 patients. Etiologically, 71.4% cases consisted of actinomycotic mycetoma and 28.6% of cases were caused by fungi (eumycetoma). Confirmation of causative agent was done on gram staining, ZN staining, KOH examination and histopathology. However, species identification was not done due to non-availability in our center. Radiological studies were normal in 28% cases, 2 patient demonstrated soft tissue swelling, lytic lesions with focal erosions/scalloping were seen in 2 patients; and soft tissue radiopacity with sclerosis, conglomerate of hypoechoic nodules and dot in a circle appearance was seen in one patient. All cases of actinomycetoma were started on a modified Welsch regimen and cases of eumycotic mycetoma were started on itraconazole. All cases demonstrated significant improvement at 3 months follow up, assessed clinically and radiologically.
Conclusion
Traditionally eumycetoma is considered to be more common in north India and actinomycetoma is predominant in south India. However, by reporting the contrasting findings, elucidating disease characteristics, associated risk factors and causative agents in this specific geographical context, our study may shed light on changing pathogen profile, to facilitate better management, prevention and control strategies for this deforming granulomatous infection.
Abstract 050 ASPICON 2024 |August 22 -25 | 2024 |
Performance Evaluation of Disk Diffusion Test Directly from Positive Blood Culture Broth for Gram negative Bacteremia – a Step Towards Antimicrobial Stewardship
Chetana Nandaniya*, Rupal Patel, Chirag Modi, Naimika Patel
Department of Microbiology, Pramukhswami Medical college, Bhaikaka University, Karamsad, Gujarat-388325, India.
* Presenting author:-: chetananandaniya07@gmail.com
Background
Performing & reporting Direct Susceptibility Testing (DST) from positive blood culture broth will help in the management of critically ill patients with sepsis. However, published studies mention that categorial agreement (CA) between direct susceptibility testing from-blood culture by disk diffusion & disk diffusion from colonies may vary between different laboratories. Therefore, a present study was conducted to determine categorical agreement (CA) and very major error (VME), major error (ME) & minor error (minE) of DST in comparison to the reference method.
Methodology
A retrospective observational study from February 2023 – May 2024 was conducted after Institutional Ethics Committee approval. DST (as per CLSI guidelines) results of Enterobacterales and non-fermenters (Pseudomonas aeruginosa & Acinetobacter spp.) were compared with reference AST method (Vitek-2 Compact & manual disk diffusion) done from colonies. CA and various types of errors of DST were evaluated. As per FDA, acceptable cut off for CA is >=90% and ME <3%. For VME, the upper limit of 95% confidence interval should be <7.5%.
Result
A total of 225 isolates were tested for 1186 antimicrobial agents. Overall CA was 94.10% (1116/1186). Non-fermenters showed better CA of 96.38% (133/138) compared to enterobacterales which showed CA of 93.80% (983/1048). A total of 2.53 % minE (30/1186), 6.43 % ME (29/451), and 1.51 %VME (11/727) were observed. Enterobacterales showed less numbers of minE as compared to nonfermenters (2.39% vs 3.62%). ME and VME were not observed in non-fermenters, however, enterobacteriales showed 2.77% ME, and 1.05% VME. In Enterobacteriaceae, maximum ME & VME errors were seen with aztreonam (9/151, 16.39%) and ceftazidime (5/148, 4.35%) respectively.
Conclusion
DST from positive blood culture broth showed a good categorical agreement and range bound errors with reference method. DST can be confidently implemented for patient’s reporting at our institute. In Enterobacterales, DST results of ceftazidime should be reported with caution.
Abstract 051 ASPICON 2024 |August 22 -25 | 2024 |
Antimicrobial and Diagnostic Stewardship of a Novel Beta Lactam/Beta- Lactamase Inhibitor in Extensively Drug-Resistant Gram-Negative Pathogens: Establishing the Realm of Promise
Debasish Biswal1*, Maitrayee Narayan2 , Sarita Mohapatra2 , Hitender Gautam2 , Benu Dhawan2 , Bimal Kumar Das2 , Naveet Wig3 , Seema Sood2
1- Department of Microbiology, Amrita Institute of Medical Sciences and ResearchCentre, Faridabad, Haryana, India
2- Department of Microbiology, All India Institute of Medical Sciences, NewDelhi, India
3- Department of Medicine, All India Institute of Medical Sciences, New Delhi, India
* Presenting author:-: debasishbiswal138@gmail.com
Background
Carbapenem…resistant Enterobacterales and Pseudomonas aeruginosa, producing metallo- beta-lactamases, are a potential nosocomial threat. The combination of aztreonam (ATM) with ceftazidime-avibactam (CZA) is a possible therapeutic approach. However, rising resistance and lack of an approved and feasible testing method of synergy is worrisome. The study aimed to evaluate the synergy and rapid detection of carbapenemases.
Material & Methodology
50 extensively drug-resistant (XDR) isolates of Enterobacterales and Pseudomonas aeruginosa were selected. Synergy between ATM and CZA was assessed using the disk stacking method, by placing one disk each of ceftazidime, CZA, ATM and stacked disks of CZA over ATM onto a cultured Muller Hinton agar plate. Positive synergy was defined as individual resistance to both CZA and ATM but susceptible to the combination. Carbapenemases were determined in isolates exhibiting positive synergy by immuno- chromatographic based methods.
Result
Klebsiella pneumoniae, Escherichia coli, Pseudomonas aeruginosa and Klebsiellaaerogenes accounted for 60% (30/50), 22% (11/50), 16% (8/50), and one isolate respectively. Overall, positive synergy was observed in 40% (20/50) of the isolates, maximum in Escherichia coli (54.5%; 6/11), followed by Klebsiella pneumoniae (40%; 12/30), Pseudomonas aeruginosa (12.5%; 1/8), and the lone isolate of Klebsiella aerogenes. NDM was the predominant carbapenemase (50%; 10/20), followed by its co- expression with OXA-48 (25%; 5/20), OXA-48 alone (15%; 3/20), and no carbapenemase in two isolates. Clinical response to the synergy along with microbiological clearance was observed in 75% (15/20) of the patients
Conclusion
Albeit limitations, Disc stacking method, being economic, can be employed in clinical microbiology laboratories in resource limited settings, lacking rapid molecular diagnostic systems. The rapid reporting of synergy results enabled clinicians to tailor treatments. This further empowered in improvement of patient outcome, reduced duration of hospital stay, optimal usage of antibiotics and reduction in antimicrobial resistance. This helped in improvement of existing antimicrobial and diagnostic stewardship practices.
Abstract 052 ASPICON 2024 |August 22 -25 | 2024 |
A Longitudinal Study of Antimicrobial Resistance Dynamics in Pseudomonas Aeruginosa – Implications in Treatment Strategies
Kanugula Harika*, Swathi Suravaram, Abdul Asma mohed
Department of Microbiology, ESIC Super Speciality Hospital, Hyderabad, Telangana, 500038, India
* Presenting author:– harikakanugula424@gmail.com
Background
Pseudomonas aeruginosa is a significant pathogen known for its resistance to multiple antibiotics, posing a challenge in both adult and pediatric patient populations. This study aims to analyze the antimicrobial susceptibility testing (AST) patterns of P. aeruginosa isolates, focusing on differences between adult and pediatric populations, temporal trends and burden of multidrug resistant (MDR) isolates.
Methodology
The present study was conducted from 2021 to 2024 at a super-speciality government teaching hospital with medical and surgical departments. Samples were collected and processed as per clinical requests, and those showing growth were analyzed using an automated identification and antibiotic susceptibility test analyzer, following CLSI M-100 guidelines. Samples growing Pseudomonas aeruginosa were included, excluding repeat samples from the same patient. Colistin resistance was confirmed using colistin broth disc elution (CBDE) and compared with automated analyzer results. Suitable antibiotics for treatment were evaluated based on CLSI M39 guidelines.
Result
In the current study, Pseudomonas aeruginosa showed varying susceptibility rates to different antibiotics ranging from 43.85% to 54.68%in adults and 41.3% to 49.32% in pediatric populations. MDR isolates were 32.8% in total with 43.2%, 12.5%, 22.5% and 22.1% from urine, blood, respiratory and exudate samples. MDR rates increased from 2021 to 2023, reaching 43.6%. Colistin susceptibility rates were relatively high with 84.45% in adults, 90.41% in paediatric population and ranged from 79% to 93% across samples. There was a discrepancy of 14.9% between automated and CBDE methods for detection of colistin resistance. All antibiotics except colistin show less than 60% susceptibility, making higher antibiotics or combinations necessary for treatment..
Conclusion
This study highlights the increasing multidrug resistance in Pseudomonas aeruginosa, necessitating tailored treatment and enhanced surveillance. While colistin remains effective, its resistance requires ongoing monitoring. Effective antibiotic stewardship is crucial to managing these infections, especially in pediatric patients.
Abstract 053 ASPICON 2024 |August 22 -25 | 2024 |
Randomized Comparative Study of Novel Teaching-Learning Methods Versus Conventional Pedagogy in Educating Phase II Mbbs Students on Different Aspects of Antimicrobial Use
Tushar Chauhan*, Puneet Kaur, Navjot Kaur, Anjleen Kaur, Jasbir Singh
Department of Pharmacology, Government Medical College, Patiala, India.
* Presenting author:– drchauhantushar1996@gmail.com
Background
Medical undergraduates are introduced to/(taught) the field of antimicrobials as a part of Pharmacology curriculum in 2nd year of MBBS. Implementation of effective teaching learning methods during this phase can better equip the future healthcare professionals to acquire necessary knowledge and skills to practice rational use of antimicrobials as standalone physicians. The present work aims to compare the novel teaching-learning methods against the conventional pedagogy on various aspects of antimicrobial use.
Material & Methodology
A randomised comparative study will be conducted among the phase II MBBS students after obtaining approval from the Institute Ethics Committee. After receiving written informed consent, the students will be randomly allocated to one of two groups: control group (using conventional pedagogy i.e. didactic lecture-based learning) or experimental group (using novel teaching-learning methods). A pretest will be administered to both the groups to have baseline assessment of the knowledge of the topic. After completion of respective teaching-learning sessions, a post-test (immediately after the session) will be administered and scores will be calculated. In addition, students’ feedback regarding novel teaching-learning methods will be obtained with the help of a post intervention survey. Data will be analysed using descriptive statistics and student’s t-test wherever appropriate.
Result & Conclusion
The knowledge gain will be determined by comparing pre-test and post-test mean scores(+SD) obtained by both the groups after the teaching sessions. Further, two groups will be compared to assess if the experimental group outperforms the control group. The feedback of students will be utilized for improving the teaching strategies in future.
Abstract 054 ASPICON 2024 |August 22 -25 | 2024 |
Comparison of Bacteriological Profile and Resistance Pattern in Two Consecutive Years in a Tertiary Care Hospital
U. Soniya Soundari*, Prerna Aggarwal, Anupam Berwal
Department of Microbiology, KCGMC, Karnal, India.
* Presenting author:– soniyasuriyan@gmail.com
Background
Medical undergraduates are introduced to/(taught) the field of antimicrobials as a part of Pharmacology curriculum in 2nd year of MBBS. Implementation of effective teaching learning methods during this phase can better equip the future healthcare professionals to acquire necessary knowledge and skills to practice rational use of antimicrobials as standalone physicians. The present work aims to compare the novel teaching-learning methods against the conventional pedagogy on various aspects of antimicrobial use.
Methodology
The bacteriology data of the past two years was collected, analysed and compared.
Result
Although the profile of bacteria isolated was largely the same in 2022 and 2023, there was a slight decrease in the number of Klebsiella species and Acinetobacter species isolated. There was a twofold rise in sample positivity from ICUs. The percentage of Escherichia coli isolated from urine specimens increased from 49% to 59% and Staphylococcus aureus from soft tissue and body fluid specimens increased from 34% to 40%. However, the percentage of Pseudomonas aeruginosa from respiratory samples decreased from 38% to 29%. There was an increase in the percentage of multi-drug resistance (MDR) isolates from 46.5% in 2022 to 57.9% in 2023. These include increased MDR strains of E. coli, Klebsiella species, P. aeruginosa and Acinetobacter species. Percentage of MRSA increased from 50% to 65.9% in the consecutive year.
Conclusion
The practices of infection control and awareness of prudent use of antibiotics needs to be made more stringent to curb the upward trend in frequency of MDR bacteria isolated.
Abstract 055 ASPICON 2024 |August 22 -25 | 2024 |
Understanding Diabetic Foot Infections: Microbiological Insights and Clinical Implications
Nitish Sharma*
Department of Orthopaedics, GMC Udhampur(J&K), India
* Presenting author:– Nitish.sharm3@gmail.com
Background
Diabetic foot infection denotes a serious complication of diabetes, characterized by microbial invasion into foot tissues. Symptoms range from localized inflammation to severe ulceration and tissue necrosis, potentially leading to limb amputation if left untreated. Most moderate-to-severe diabetic foot infections (DFIs) require hospitalization with urgent surgical approach and administration of empiric antibiotherapy. To ensure optimal antibiotic coverage, regular microbiological background updates are imperative.
Aim of this study is to characterize the microbiological profile and the antibiotic sensitivity pattern of the DFI causative pathogens.per antimicrobial agents according to culture sensitivity.
Methodology
Our study is a prospective study in which 101 patients of moderate to severe Diabetic foot infection were admitted in Orthopaedic deptt of a tertiary care hospital of North India over a period of 3 years. Microbiological cultures from deep tissues were taken and sent to the microbiology deptt of the centre where Gram staining, Culture and corresponding antibiotic sensitivities were performed. Specific antibiotics were administered subsequently along with debridement of the diabetic ulcers as per required.
Result
A total of 101 patients were included in the study over the period of 3 years. The mean age of patients was 57.1 ± 9.1 years. There were more males (64.4%), mostly with type 2 diabetes (99%), with a median duration of 9 years. Their median blood sugar on admission was 246 mg/dL. Five percent of patients died and 23% had a major amputation. Twenty-eight germs were isolated in
different cultures. A total of 60.0% of the isolates were Gram-positive bacteria and 40 % were Gram-negative bacteria. Staphylococcus aureus was the most common Gram-positive aerobe bacteria, followed by Enterococcus spp and Streptococcus spp. Gram Negative organisms were Pseudomonas aeruginosa , Proteus spp , Escherichia coli , Enterobacter spp. and Klebsiella spp. Considering the AST data and the comparison established between recommended empiric antibiotics, there are some highlights to address. Excluding MRSA, Gram-positive bacteria represented 45% of the pathogens recorded, and almost all of them were sensitive to amoxicillin/clavulanic acid and piperacillin/ tazobactam. Gram-negative bacteria showed a high resistance to amoxicillin-clavulanic acid, fluoroquinolones, and gentamicin. They were susceptible to imipenem, and amikacin, and showed moderate susceptibility to third-generation cephalosporins.
Conclusion
Gram-positive bacteria are still the main causative pathogens of Diabetic foot infections.. Our study highlights piperacillin/tazobactam as the best first-line empirical antibiotic option to treat severe DFI. Along with the antibiotic administration, debridement of the infected diabetic wound is also to be emphasized for better antibiotic action.
Abstract 056 ASPICON 2024 |August 22 -25 | 2024 |
In Vitro Activity of Aztreonam in Combination with Ceftazidime – Avibactam, Piperacillin – Tazobactam, Cefoperazone – Sulbactam and Amoxicillin – Clavulanate in NDM producing Escherichia coli, Klebsiella pneumoniae and Pseudomonas aeruginosa from Bloodstream Infections
Gaurav Salunke*, Santosh Harkal, Sanjay Biswas, Jyoti Sinol
Department of Microbiology, Tata Memorial Hospital, HBNI University, Mumbai, India.
* Presenting author:– drgsalunke@yahoo.com
Background
Multidrug-resistant (MDR) Gram-negative organisms are a major health concern due to lack of effective therapy. Emergence of NDM producing organisms further magnifies the problem. In this context, combination therapy of Aztreonam with other antimicrobials may have potential in treating these pathogens. Unfortunately, there are limited data regarding these combinations.
Methodology
51 NDM producing clinical isolates of Escherichia coli, Klebsiella pneumoniae and Pseudomonas aeruginosa being the potential pathogen in bacterial septicemia were included in this study. The potential for synergy was evaluated via the broth disc elution method. The disk content/CA-MHB ratio (4/8 μg/mL ATM) was purposefully chosen as the ATM concentration would be around the CLSI susceptibility breakpoint for both the Enterobacteriales (4 μg/mL) and P. aeruginosa (8 μg/mL) strains. After overnight incubation, the tubes were assessed for no growth (susceptible) or growth (not susceptible) based on the breakpoints
Result
According to CLSI breakpoints, Aztreonam susceptibility was fully restored for 50%, 22.7%, 13.6% and 4.5% of the NDM producing E. coli isolates when combined with Ceftazidime – Avibactam, Amoxicillin – Clavulanate, Piperacillin – Tazobactam and Cefoperazone – Sulbactam respectively. In K. pneumoniae and P. aeruginosa, the Aztreonam + Ceftazidime – Avibactam combination was the most potent in 74% and 100% isolates respectively.
Conclusion
Our findings show that overall, Aztreonam + Ceftazidime – Avibactam was the most potent combination to treat infections caused by NDM producers. Aztreonam in combination with other BL/BLI has potential for therapeutic options in difficult to treat pathogens but further evaluation of is warranted.
Abstract 057 ASPICON 2024 |August 22 -25 | 2024 |
A Serial Point Prevalence Survey (PPS) of Antimicrobial Use Amongst Admitted Patients in Critical Care Settings of a Tertiary Care Teaching Hospital in Raipur District
Nikunj R. Agrawal*, Nitin R. Gaikwad, Yogendra N. Keche
Department of Pharmacology, All India Institute of Medical Sciences, Raipur, India.
* Presenting author:– nikunj.agrawal178@gmail.com
Background
Antimicrobial resistance (AMR) poses a significant global health threat exacerbated by inappropriate antimicrobial use. The WHO predicts AMR could cause up to 10 million deaths annually by 2050, primarily due to misuse. In India, antimicrobial consumption surged by 103% from 2000 to 2015, emphasizing the urgent need for effective antimicrobial stewardship programs (AMSPs).Conducting point prevalence surveys (PPSs) in India’s resource-limited settings is challenging, resulting in sparse data on antimicrobial use.This study aimed to establish baseline data on antimicrobial utilization in critical care settings through serial PPSs at AIIMS Raipur, a tertiary care teaching hospital.
Methodology
Over 12 months, data was collected monthly from June 2023 to May 2024 across nine critical care settings. The study included all patients admitted to critical care settings by 8:00 am on survey days, excluding emergency department patients and those on topical or antitubercular antimicrobials. Data on patient demographics, reasons for antimicrobial use, and therapy specifics were collected using a Google Form for Data Abstraction.
Result
A total of 908 admitted patients in nine critical care settings were surveyed in 12 months. Of these, 505 (55.61%) patients were on antimicrobials out of which 320 (63.37%) patients were on two or more antimicrobials. Out of the total antimicrobials prescribed, 79.84% of the antimicrobials were
prescribed for hospital-acquired infections followed by community acquired infections (15.02%). Antibiotic usage was highest in Critical care units (15.7%), Trauma and Emergency ICU (15.05%), and paediatric ICU (14.94%). The antimicrobials used were commonly from WHO “WATCH” category of which Piperacillin-Tazobactam was prescribed most (14.61%) followed by Meropenem and Vancomycin (11.78% each).
Conclusion
This serial PPS demonstrated crucial insights into antimicrobial prescribing patterns, essential for developing targeted AMSP strategies and reducing AMR, thereby improving patient outcomes in critical care facilities.
Abstract 058 ASPICON 2024 |August 22 -25 | 2024 |
Leveraging Antimicrobial Stewardship in Paediatric Pneumonia: An appraisal of prescription practices at a tertiary care hospital
Shariqa Qureshi1*, Ananya Arora2 ,Dhulika Dhingra3
1- Department of Clinical Microbiology and Infectious Disease, Chacha Nehru Bal Chikitsalaya, Delhi, India.
2. Ex Fellow, Paediatric Infectious Disease, Chacha Nehru Bal Chikitsalaya, Delhi, India.
3. Specialist (Paediatrics) National Institute of Tuberculosis and Respiratory diseases, Delhi, India.
* Presenting author:– drshariqa@gmail.com
Background
Community-acquired pneumonia (CAP) is a leading cause of mortality among children under five years old, particularly in developing countries such as India. Despite the predominance of viral causes for CAP, the overprescription of antibiotics remains prevalent, exacerbating antimicrobial resistance (AMR) and undermining patient care.
Objective: This study aims to evaluate the antimicrobial prescription practices for paediatric CAP in a tertiary care hospital in India. The primary objectives include assessing adherence to hospital antibiotic policies, optimizing antibiotic use, and improving patient outcomes through an antimicrobial stewardship program (AMSP).
Methodology
A prospective observational study was conducted over three months, enrolling 100 patients aged 1 month to 12 years with CAP. Participants were recruited from the paediatric emergency and wards at Chacha Nehru Bal Chikitsalya, New Delhi. Antimicrobial prescriptions were evaluated for compliance with established guidelines. Biomarkers, radiographic patterns, and microbiological tests were utilized to guide treatment and monitor adherence to AMSP protocols. The study also compared clinical outcomes between children receiving stewardship intervention versus those who did not.
Result
The study observed 51% of prescriptions non-adherent to hospital policy. Implementation of AMSP led to a noticeable reduction in inappropriate antibiotic use, with increased compliance to first-line treatments and decreased reliance on broad-spectrum antibiotics. The stewardship intervention group showed improved clinical outcomes, including reduced hospital stay duration without an increase in morbidity or mortality.
Conclusion
The findings underscore the critical need for AMSP in paediatric settings to mitigate the adverse impacts of AMR. Adherence to antibiotic guidelines can significantly enhance the quality of care for children with CAP, fostering responsible antimicrobial use and better health outcomes. This study highlights the importance of continuous education and monitoring to ensure the success of stewardship programs in improving paediatric health care.
Abstract 059 ASPICON 2024 |August 22 -25 | 2024 |
Real World Evidence on the Impact of Implementation of Antimicrobial Stewardship (AMS) Practices on Antimicrobial Resistance and Therapeutic Outcomes on a Tertiary Care Hospital of West Bengal
Raja Chakravertya*, Asim Kumar Kundu
Department of Critical Care Medicine Institute of Post Graduate Medical Education and Research. Kolkata, India.
* Presenting author:– rchakraborty20@yahoo.com
Background
The study was conducted to gather information to evaluate the extent of impact of antimicrobial stewardship (AMSP) practices on antimicrobial prescribing patterns and bacterial resistance profiles among indoor patients across ten ICU and non-ICU departments at the Institute of Postgraduate Medical Education and Research, Kolkata.
Methodology
The study protocol was submitted to the Institutional Ethics Committee of the institute and it was approved unanimously. Data from indoor patients were collected prospectively from June, 2022 till October, 2023. The use of antimicrobials was categorized as empiric, prophylactic or targeted/culture driven. The WHO-AWARE classification of antimicrobials was used to classify systemic antimicrobials being prescribed to patients. Study data was archived and analyzed using software such as SPSS 20.0 (IBM), Jamovi and Med Calc 8 (Belgium).
Result
Total number of beds covered annually was 2972 and the number of patients on antimicrobials was found to be as high as 98.57 %. Relatively higher number of patients were found to be on two or more antimicrobials predominantly from WATCH and RESERVE categories. Interestingly, among nosocomial CLABSI and CAUTI rates were 22.05 % and 22.11 % respectively with a relatively lower proportion of SSIs 0.88%. Mortality relatedness to infection was found to be 48.62 %. The overall compliance rate to hospital antibiotic policy was found to be 72. 51% while culture was sent in nearly 59% of the patients surveyed. Rationality assessment and prospective audit and feedback of antimicrobials was performed which is under analysis.
Conclusion
This preliminary study resulted in acquisition of data not only related to resistance profiles of microbial pathogens to antimicrobials but also yielded data about determinants of hospital acquired infection including surgical site infections which may aid policy makers to formulate newer antimicrobial guidelines in the state and country based on such definitive findings.
Abstract 060 ASPICON 2024 |August 22 -25 | 2024 |
Trends of Antimicrobial Resistance among Blood Isolates at a Tertiary Care Centre in North India: A Retrospective Six-Year Study
Veenu Gupta*, Rama Gupta, Menal Gupta, Jyoti Chaudhary, Manisha Aggarwal
Department of Microbiology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
* Presenting author:– vsunilgupta@rediffmail.com
Introduction
Bloodstream infections are important causes of morbidity and mortality worldwide. Candidemia is also being frequently reported and is mostly associated with immune suppression, prolonged antibiotic usage, invasive surgical procedures, intravenous devices and parenteral nutrition. The rising rates of antimicrobial resistance among pathogens in India are alarming, because of the high infection rates and poor control of antibiotic use thus antimicrobial surveillance is essential for identifying emerging resistance.
Aim: To study trends of antimicrobial resistance among blood isolates.
Materials & Methodology
This retrospective, observational study was performed in the Microbiology laboratory of a tertiary care hospital from 2018 to 2023. Blood samples from patients with suspected BSI were cultured on automated systems (BD Bactec Fx/ BactAlert 3D). Identification and antimicrobial susceptibility testing were performed on the Vitek2 system. The data was retrieved from the laboratory records and antimicrobial resistance profiles were analysed.
Result
Overall blood culture positivity of pathogenic bacteria and Candida spp was 12% (varying from 11.8% in 2018 to 11.5% in 2023), while year-wise positivity rates of candidemia was 0.68%, 0.73%, 0.82%, 0.71%, 0.50% and 0.55% from 2018 to 2023 respectively. Escherichia coli (21.5%) and Klebsiella pneumoniae (18.2%) were the predominant isolates, followed by Acinetobacter baumannii (8.9%), Staphylococcus aureus (8.3%) and
Candida spp (5.8%). Among Candida isolates, C. tropicalis was the most common followed by C. albicans and C. parapsilosis. The Gram-negative isolates showed high rates of resistance to third generation cephalosporins, β-lactam-β-lactamase inhibitor combinations and carbapenems. Methicillin-resistant S. aureus isolates increased from 67% to 83% over the six-year period, while vancomycin-resistant enterococci also escalated from 31% to 40% in 2022, with a fall to 22% in 2023. In comparison, Candida isolates showed good susceptibility to amphotericin B & echinocandins whereas increased resistance to azoles (10-25%) was observed in C. tropicalis and C. parapsilosis.
Conclusion
The study revealed that the majority of bloodstream infections were caused by Gram-negative pathogens with high rates of resistance to most antimicrobials and predominance of non-albicans Candida species. Regular monitoring of local trends of antibiotic resistance detects early shifts in susceptibility and also serves as a basis for empirical therapy, formulary decisions, and infection control practices.
Abstract 061 ASPICON 2024 |August 22 -25 | 2024 |
Emergence of Multidrug-Resistant Klebsiella pneumoniae: Antimicrobial Susceptibility Trends (2019-2023) in an Indian Tertiary Care Hospital
Shubhangi Kansal*, Archana Angrup, Neelam Taneja
Department of Medical Microbiology, Postgraduate Institute of Medical Education & Research, Chandigarh, India
* Presenting author:– shubhangi.kansal03@gmail.com
Background
The rise of multidrug-resistant (MDR) Klebsiella pneumoniae, causing nosocomial infections and significant mortality, has made it a WHO “priority pathogen.” This study examines the antimicrobial susceptibility of K. pneumoniae from pus specimens in an Indian tertiary care hospital, identifying trends in MDR spread.
Materials & Methodology
Clinically relevant isolates from culture-positive pus samples were identified using MALDI-TOF, and antimicrobial susceptibility testing (AST) was performed via Vitek2 systems. Colistin resistance was assessed using microbroth dilution as per CLSI/EUCAST guidelines. Data management and statistical analysis were conducted using WHONET and GraphPad Prism, respectively. Categorical variables were analyzed using χ2 or Fisher exact test, with Odds Ratios (ORs) and 95% Confidence Intervals (CIs) calculated.
Result
From 2019-2023, 5801 K. pneumoniae isolates (13.1%) were identified from 44,414 positive pus specimens. The prevalence of K. pneumoniae increased by 14% in 2023 compared to 2019 (p<0.05). AST showed a significant rise in carbapenem resistance, with 9.2% of isolates resistant to both carbapenems and colistin (p<0.0001). MDR K. pneumoniae was more prevalent among inpatients compared to outpatients (p<0.0001, OR: 1.817, CI: 0.7945 to 2.079). A moderate positive association was found between K. pneumoniae isolates from Medicine wards and MDR cases (p<0.0001, OR: 1.583, CI: 0.7014 to 1.786). Resistance increased significantly post-COVID-19.
Conclusion
The study revealed concerning trends in Klebsiella pneumoniae antimicrobial resistance at an Indian tertiary care hospital, with a 14% surge in prevalence by 2023. Notably, 9.2% of isolates were resistant to carbapenems and colistin. Inpatients had significantly higher rates of multidrug-resistant K. pneumoniae, highlighting the urgent need for enhanced infection control measures.
Figure 1: Increase in %R for carbapenem and colistin post COVID-19.
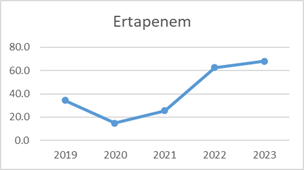

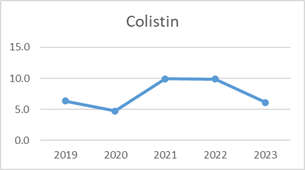
Figure 2: Increase in Carbapenem resistance K. pneumoniae isolates.
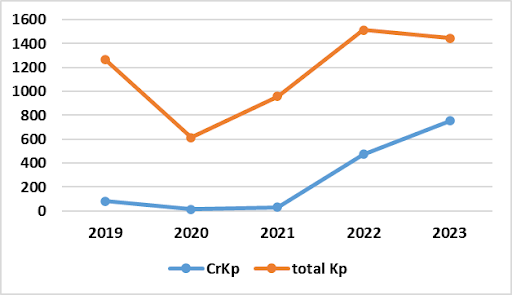
Abstract 062 ASPICON 2024 |August 22 -25 | 2024 |
To Assess Symptomatic Improvement with Prescribed Antibiotics in Uncomplicated Urinary Tract Infections (UTIs)
Sachin Kumar Sharma*, Poonam Arora
Department of Pharmacology, RMRI Bareilly India.
* Presenting author:-sachinsharma1849@gmail.com
Introduction
Antibiotics are among the most frequently prescribed medications for outpatients suffering from uncomplicated urinary tract infections.
Aims and Objectives: To assess symptomatic improvement with prescribed antibiotics in uncomplicated urinary tract infections.
Materials & Methodology
This study was conducted on 60 male patients diagnosed with uncomplicated UTI. It was an observational, follow up study. Inclusion criteria was male patients age >16 years, diagnosed as case of uncomplicated UTI based on symptoms suggestive of UTI including burning micturition, increased frequency of urination, urgency, suprapubic pain, blood in urine, cloudy urine, fever with or without chills. Exclusion Criteria was catheter associated UTI, complicated UTI cases due to stones, strictures, neurogenic bladder, recurrent UTI and previous history of surgery involving genitourinary tract.
Result
Antibiotic | Dose | Duration of therapy in days | No of Prescriptions (%) | Symptomatic Relief in no of patients (%) | Symptomatic Relief in number of days (Mean±S.D.) |
Levofloxacin | 500 mg OD | 7 | 19 (31.66% ) | 5 (26.31 % ) 5 | 5±0.63 |
Levofloxacin | 750 mg OD | 5 | 6 (10% ) | 1 (16.66 % ) | 4.5±1 |
Ofloxacin | 100 mg OD | 5 | 4 (6.66% ) | 4 (100 % ) | 5 |
Ciprofloxacin | 500 mg OD | 5 | 4 (6.66% ) | 2 (50%) | 5±0.63 |
Norfloxacin | 400 mg OD | 7 | 9 (15%) | 9 (100%) | 3 |
Nitrofurantoin | 100 mg OD | 7 | 18 (30% ) | 14 (77.77% ) | 4.2±2.11 |
Interpretation
In this study, we found that Levofloxacin and Nitrofurantoin are the two most commonly prescribed antibiotics for uncomplicated UTI patients. Nitrofurantoin 100 mg BD provides symptomatic relief earlier than other antibiotics which make it a better choice for such patients.
Abstract 063 ASPICON 2024 |August 22 -25 | 2024 |
The Novel Automated Multiplex Pcr Respiratory Panel a Boon or Bane? For Stewardship Practices, An Experience from Dedicated Liver Hospital in North India
Rishiraj bhatt1* ,Vikas khillan2 ,Pratibha Kale3 , Rakhi Maiwall4
1.Department of Clinical Microbiology, AIIMS New Delhi
2. Department of Microbiology and Infection Control, ILBS Vasantkunj ,New Delhi
3. Department of Microbiology and Infection Control, ILBS Vasantkunj ,New Delhi
4. Department of Hepatology,ILBS Vasntkunj ,New Delhi
* Presenting author:-Doctorrishi87@gmail.com
Background
Ven$llator associated pneumonia [VAP] is second most common HAI in ICU se:ngs.The diagnosis of VAP is complex and requires correla$on between Clinical ,radiological and Microbiological criteria. The CDC supports semi quantitative reporting for respiratory samples sent for culture to rule out colonization .The novel mul$plex PCR pneumonia panel has a TAT of 1 hour which when compared to Culture of respiratory specimens require minimum 48 hrs.The role of respiratory sample culture in stewardship prac$ces is well known because of CDC semi quantitative threshold values but role of This Novel mul$plex Respiratory PCR is not well described in studies and need further evaluation, secondly the Automated PCR gives its final result in unit Bin copies/ml which is totally different from culture result unit CFU/ml leading to confusion for trea$ng physician in significance of pathogen as a coloniser or as a true pathogen
Materials & Methodology
• Study Type : Retrospective observational study
• Study period : September 2020 – Dec2020
• Study population : Liver disease patients of all age groups with clinically suspected lower respiratory tract bacterial infection admitted to Liver CICU
• Sample size : 157
• All respiratory samples received in microbiology lab were subjected to culture as well as PCR and results were compared at last
Result
• Majority of 10^5 culture positive isolates were identified by PNP as 10^7 and 10^6 bins
• Both PNP and culture were +ve in 19.1% cases
• Both PNP and culture were –ve in 51% cases
• Genotypic resistance detected by PNP matched Phenotypic resistance detected by VITEK in 100% cases in case of gram neg bacteria
• MeC-A/C gene were detected by PNP in all cases of MRSA detection by VITEK[PHENOTYPIC]
• Additional 28.6% gain was seen in diagnosis of bacterial isolates which were negative on culture
Conclusion
Novel multiplex respiratory PCR is a great tool for early detection of MDR pathogen causing pneumonia and aids in stewardship practices.
Abstract 064 ASPICON 2024 |August 22 -25 | 2024 |
Evaluating the Efficacy of Ceftazidime-Avibactam and Aztreonam synergistic combination among Carbapenem Resistant E. coli and Klebsiella spp.
Barasha Das*, Arti Agrawal, Pragya Shakya, Archana
Department of Microbiology, S.N Medical College, Agra (U.P), India.
* Presenting author:-barashadas@gmail.com
Introduction
Carbapenems are preferred over other types of antimicrobial agents in treating invasive or severe infections due to their concentration-independent killing effect on the infecting bacteria. Carbapenem resistance in Gram-negative bacteria has been increasingly encountered in healthcare-associated infections in India. Ceftazidime-avibactam (CZA) and Aztreonam (ATM) combination therapy is used specifically to target infections caused by Metallo-beta-lactamase (MBL) producing Carbapenem-resistant Enterobacteriaceae (CRE). When combined, Ceftazidime-avibactam protects Aztreonam from hydrolysis by non-MBL beta lactamases. Aztreonam remains active against the MBLs, providing a synergistic effect. This study aimed to evaluate the synergistic effect of Ceftazidimeavibactam and Aztreonam combination in Carbapenem resistant Enterobacteriaceae.
Materials & Methodology
Carbapenem – resistant Enterobacterales were included in a study conducted in the Department of Microbiology, S.N. Medical College, Agra. The isolates were collected from different sources such as urine, blood, pus, respiratory specimens like sputum, bronchoalveolar lavage fluid and other body fluids. Samples received were processed by conventional methods for identification. Gram-negative isolates obtained were subjected to antimicrobial susceptibility testing by the Kirby–Bauer disc diffusion method using the following discs amikacin, ceftazidime, cefepime, ciprofloxacin, imipenem, cefoperazone/sulbactam, piperacillin/tazobactam, co-trimoxazole, ceftazidime/ avibactam and aztreonam.
Result
Out of 293 Carbapenem-resistant isolates, 71.33% are Klebsiella spp and 28.66% are E. coli. Synergy test among E. coli and Klebsiella spp is under process. Out of 293 Carbapenem resistant Enterobacteriaceae studied, 78% isolates showed resistance to piperacillin-tazobactam, 47% isolates are resistant to amikacin, 55% isolates are resistant to cotrimoxazole.
Conclusion
The use of Ceftazidime-avibactam together with Aztreonam is a potentially suitable combination for the treatment of Carbapenemase-producing microorganisms and is available in clinical laboratories. As the combination has less side effects so the in vivo efficacy of this combination needs to be evaluated.
Abstract 065 ASPICON 2024 |August 22 -25 | 2024 |
Emergence of Multidrug-Resistant Non-fermentating Gram Negative Bacilli and Carbapenem Resistant Acinetobacter baumannii (CRAB) in a Tertiary Care Hospital of Northern India
Ekta Rawat*, Pragya Shakya, Arti Agrawal, Ankur Goyal
Sarojini Naidu Medical College, Agra,Uttar Pradesh, India.
* Presenting author:-drekta0509@gmail.com
Background and Objective
Nonfermenting gram negative bacilli (NFGNB) are now emerging as important nosocomial pathogens causing hospital-acquired infections and opportunistic infections. This study aimed to determine the antibiotic susceptibility pattern of NF-GNB isolated from all clinical samples to estimate the prevalence of Multidrug resistant NF-GNB and to screen for Carbapenem resistant Acinetobacter baumannii (CRAB) strains.
Materials & Methodology
An observational study with a cross-sectional design was conducted between September 2023 to May 2024 in the Department of Microbiology, S.N. Medical College Agra. We identified MDR NF-GNB from clinical samples using standard procedures and antimicrobial susceptibility testing done by Kirby Bauer disc diffusion method and MBL detection by EDTA double disc synergy test by using commercially available discs (Hi-media) i.e. Amoxicillin/clavulanic acid (20/10mcg), Piperacillin, (100mcg), Piperacillin/tazobactam (100/10mcg), Ceftazidime (30mcg), Cefepime(30mcg), Trimethoprim/sulfamethoxazole (1.25/23.75mcg), Ciprofloxacin(5mcg), Levofloxacin (5mcg), Amikacin (30mcg), Meropenem (10mcg), Imipenem (10mcg), Polymyxin B (300 mcg), Doxycycline (30mcg), Co-trimoxazole (25mcg), Tobramycin (10mcg), Minocycline (30mcg), Colistin (10mcg), Tigecycline (15mcg).
Result
A total of 270 MDR-NFGNB were isolated in 700 non fermenters gram negative bacilli and most common samples were blood (n= 90, 33.3%) followed by pus (n=74 ,27.4%). Among MDR-NFGNB the most common organisms were Pseudomonas aeruginosa (n=126,46.6%), followed by Burkholderia cepacia complex (n=68,25.1%), Acinetobacter baumannii (n=67,24.8%) and others. The susceptibility pattern of these isolates were piperacillin-tazobactam (45.1%), imipenem (39.2%), aztreonam (18.5%), amikacin (17.4%), ceftazidime (14.0%), ciprofloxacin (10.7%), doxycycline (8.8%), cefepime (7.4%), cotrimoxazole (5.5%).Maximum MBL production was obtained in Acinetobacter spp. followed by Pseudomonas aeruginosa and the Carbapenem resistant Acinetobacter baumannii were (n=42,55%).
Conclusion
Since these organisms have great potential to survive in the hospital environment, improved antibiotic stewardship and infection control measures are required to prevent the emergence and spread of drug-resistant NFGNB in healthcare settings.
Abstract 066 ASPICON 2024 |August 22 -25 | 2024 |
From Blueprints to Reality: Journey of a Clinical Pharmacologist Post-3rd ASPICON
Khushboo Bisht 1,2*, Sanjeev Kumar Singh1 , Minakshi Dhar2 , Prasan Kumar Panda2 , Debasish Biswal1
1- Amrita Institute of Medical Sciences and Research Centre, Faridabad, Haryana, India.
2- All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
* Presenting author:-khushboobisht12@gmail.com
Introduction
Antimicrobial resistance (AMR) poses a significant threat to global public health, largely driven by the misuse and overuse of antibiotics. Antimicrobial Stewardship (AMS) programs aim to optimize antibiotic use, enhance patient outcomes, and reduce AMR. This study details the experiences of a clinical pharmacologist in implementing AMS interventions in two tertiary care hospitals, focusing on the strategies employed and their impact on antibiotic use and patient outcomes.
Methodology
The AMS program, led by a clinical pharmacologist, was implemented over a one-year period at two different tertiary care hospitals. Key interventions included: a) PostPrescription Review and Feedback: Reviewing ongoing antibiotic therapies and providing recommendations based on patient progress and microbiological data. b) Educational Initiatives: Conducting workshops, case discussions, and disseminating guidelines to promote judicious antibiotic use. c) Multidisciplinary Collaboration: Participating in rounds and collaborating with infectious disease specialists, microbiologists, and nursing staff. Data on antibiotic usage, compliance with guidelines, incidence of C. difficile infections, and patient outcomes were collected and analyzed.
Result
AMS interventions led to a 20% decrease in continued use of broad-spectrum antibiotics and an increase in de-escalation practices. Compliance with evidence-based guidelines increased from 60% to 85%.
Additionally, the average hospital stay was reduced by 2 days, with a corresponding decrease in antibiotic-related adverse events.
Conclusion
AMS interventions, including post-prescription review, educational initiatives, and multidisciplinary collaboration, significantly optimized antibiotic use and improved patient outcomes. Continuous monitoring and collaboration are essential for sustaining AMS benefits and addressing emerging challenges.
Abstract 067 ASPICON 2024 |August 22 -25 | 2024 |
Prevalence of Dengue and Leptospirosis Co-infection at Tertiary Care Hospital, Mumbai
Jyoti Bala*, Nupur Chandra, Tejasvini Sonavane, Meghna Palawer, Nilma Hirani
Department of Microbiology, Grant Government Medical College & Sir JJ Hospital, Mumbai, India.
* Presenting author:– bala123jyoti@gmail.com
Background
Dengue and Leptospirosis are both infectious diseases and thus pose a threat to public health, especially in tropical regions like Mumbai. During monsoon, the incidence of the infections is widespread. Due to concurrent transmission, the possibility of co-infection may increase. The severity of the infection is heightened because of the concomitant infection. Despite this, there are not many studies available to address the severity of co-infection.
Aim: To determine the prevalence of Dengue and Leptospirosis co-infection, by Dengue NS1 antigen and IgM, Leptospirosis IgM ELISA.
Methodology
Retrospective observational laboratory-based study has been conducted over a period of 6 months in tertiary care hospital, Mumbai. A total of 3372 serum samples were received from patients with acute febrile illness and examined for dengue NS1 and IgM. Positive Dengue samples were additionally tested for IgM antibody against Leptospirosis by ELISA and co-infection was diagnosed.
Result
Out of 3372 received serum samples, 418 (12.39%) found positive for Dengue and among these 86 were co-infected with prevalence of 2.55 %. 19 cases of co-infection reported in the month of October and November.
Conclusion
These findings added a new dimension in the management of Dengue and Leptospirosis. The possibility of these concurrent infections should be considered especially in endemic areas for early diagnosis and proper treatment, thereby decreasing the mortality.
Abstract 068 ASPICON 2024 |August 22 -25 | 2024 |
A Quality Improvement Initiative to Improve the Implementation Fidelity to Institutional Surgical Antibiotic Prophylaxis Policy
Sadia Khan1*, Sharmila Sengupta1, Meenakshi Chakraborty2, Aparna Chakravarty3
Departments of Microbiology1, Infection Prevention2 & Pediatric Infectious Diseases3, Amrita School of Medicine, Faridabad, India.
* Presenting author:– sadia.khan@fbd.amrita.edu
Background
A Quality Improvement (QI) initiative aimed at enhancing infection control and reducing Surgical Site Infections (SSI) was undertaken at our institute. A significant component of this initiative focused on improving compliance with Surgical Antibiotic Prophylaxis (SAP) guidelines due to observed non-uniform practices across surgical departments.
Methodology
The QI project employed the Plan-Do-Study-Act (PDSA) methodology to systematically address SAP compliance. Initial steps included a gap analysis conducted by the Infection Prevention and Control (IPC) and Antimicrobial Stewardship Program (AMSP) teams, leading to the development and dissemination of institutional SAP guidelines. Data was collected on SAP practices, specifically focusing on the choice, dose, and timing of antibiotic administration, and compliance was audited monthly. The project aimed to increase SAP compliance to over 80% by April 2024, using targeted education, training, and continuous feedback mechanisms.
Result
The initial audit in July 2023 revealed varied compliance with SAP guidelines, with significant deviations in antibiotic choice, dose, and timing. Following the implementation of the QI interventions, compliance rates improved notably by April 2024. The proportion of surgeries with the correct antibiotic choice increased from 75% to 100%, the correct dose from 75% to 100%, and the correct timing from 50% to 100%. Correspondingly, the rate of SSIs decreased from
7.8% in November 2022 to 3.9% by April 2024, demonstrating the effectiveness of the QI initiative.
Conclusion
The QI project successfully improved compliance with SAP guidelines through structured interventions, significantly reducing SSI rates. Continuous monitoring, feedback, and iterative adjustments to the implementation strategies were crucial to achieving these outcomes. The initiative underscores the importance of a collaborative & multidisciplinary approach in driving quality improvements in surgical practices and infection control. Future steps will focus on sustaining high compliance levels and further reducing postoperative antibiotic use in non justified cases.
Abstract 069 ASPICON 2024 |August 22 -25 | 2024 |
Case of Multifocal Abscesses in Uncontrolled Diabetes
Adithya Lingala, Adarsh Patil, Ishan Verma, Nilesh Kamble*, Sunita Kumbhalkar
Department of General Medicine, All India Institute of Medical Sciences, Nagpur, India.
*Presenting author:-nils0279@gmail.com
Abstract
Burkholderia cepacia is a pathogen usually causing infection in immunocompromised, uncontrolled Diabetes. It is also associated with infections in patients with underlying lung disease, such as cystic fibrosis and chronic granulomatous disease. Burkholderia infection mimics tuberculosis closely due to a similar clinical profile.
We present a case of disseminated B. cepacia infection in a 42 years old male patient with newly detected Uncontrolled type 2 diabetes mellitus and ischemic heart disease.
Patient was symptomatic for 1 month with intermittent low grade fever, chest discomfort and intermittent episodes of diaphoresis and palpitations. He also complained of burning micturition for 15 days, associated with incomplete voiding. He had a well defined, fleshy ulcerated lesion with purulent discharge over his left tibial tuberosity. Investigations were suggestive of neutrophilic leukocytosis anemia of chronic disease, mild transaminitis, HbA1c of 12.1% and elevated inflammatory markers – ESR, CRP, Ferritin and Procalcitonin was also elevated. Urine routine examination had 25-30 pus cells/hpf, albeit the cultures were sterile on serial 3 samples. USG revealed splenic abscess with prostatomegaly, hence CT Thorax and Abdomen-pelvis was done and was suggestive of Splenic, Prostatic abscess and loculated, septated collections in anterior and middle mediastinum encasing the ascending aorta, arch of aorta, the SVC and right atrium. There were also multiple subcentimeter mesenteric, retroperitoneal, inguinal and mediastinal reactive Lymph nodes.
CT guided Pus was drained from prostatic abscess, and pus from the ulcer revealed the growth of Burkholderia cepecia sensitive to Meropenem and cotrimoxazole which were started as per the indicated preferred regimen for 4 weeks to which the patient dramatically responded. Cotrimoxazole was further continued for 3 months and the patient has clinicoradiological resolution on follow up.
Bulkholderia is a great mimic of tuberculosis especially in endemic areas. It affects the immunocompromised individuals, and also specifically in poorly controlled Diabetes Mellitus and can cause multitude of clinical manifestations including disseminated abscesses as was in our case. Clinical suspicion of Melioidosis can prompt early diagnosis and treatment.
Abstract 070 ASPICON 2024 |August 22 -25 | 2024 |
The Crucial but Unrecognized Role of Nurses in Antimicrobial Stewardship: A Systematic Review on the Challenges and Opportunities
Asheema Khosla*
Department of Pharmacology, PGIMER
* Presenting author:-asheema.khosla@gmail.com
Introduction
The widespread misuse of antimicrobials has led to the development of resistance in bacteria, viruses, fungi and parasites. Antimicrobial resistance is a worldwide concern which has contributed to national and global health crises, and with the global threat of AMR emergence there should be wider involvement between the multidisciplinary healthcare team. This article proposes possible ways of engagement of Nurses as Antimicrobial Stewards.
Objective: The aim of this evaluation is to determine the challenges and opportunities for the nurse role in the antimicrobial stewardship.
Methodology
PubMed/MEDLINE, EMBASE and Web of Science were searched for articles in English. The search strategy included indexing (MeSH) terms and text words for nurses, antimicrobial stewardship, antimicrobial resistance, antimicrobial stewardship programme and training and curriculum. Internet search engines were used to search the grey literature for reports, qualitative studies, cross-sectional studies and Randomized controlled trials. Rayyan® was used to organize and extract data.
Result
Out of 618 initial hits, 61 articles were included for data extraction. 219 duplicates were removed. Majority of the studies were Surveys (44%) followed by Qualitative studies (21%), Cross-Sectional studies (5%) and RCTs (1%). Studies were included from both LIMCs (46%) and HICs (53%) specifically from the Europe region. AMS challenges should be addressed by collaborative and methodical approach, aiming to implement AMSP in an effective manner.
The studies have attempted to evaluate the impact of educational initiatives on AMS practices for nursing students. It is evident from various studies that their curriculum lacks Education and proper training on AMS. Numerous surveys, interviews were conducted to assess the knowledge, attitude and perceptions of nursing students, clinical nurses and staff nurses. They were aware of their deficiency, the majority affirmed that the current curriculum of nursing degree should have more training on antibiotics and infection control because nursing staff plays a critical role in the rational use of antibiotics, so their training can be a key in fighting the antibiotic resistance. Furthermore, Inter-professional hierarchy and lack of cooperation by the prescribers was a major area of concern in the implementation of AMS. A number of potential interventions are identified that may prevent or mitigate these problems. Aside from preparing, administering and monitoring the effects of antimicrobials, nurses are involved in coordinating care, clinical assessment, taking specimens, monitoring patient progress and reporting adverse events, all of which offer opportunities to influence antimicrobial prescribing.
Conclusion
The inclusion of Nurses in Antimicrobial Stewardship is pivotal and through proper education and training they can have significant impact on the antimicrobial resistance patterns and can contribute in reducing the AMR burden.
Abstract 071 ASPICON 2024 |August 22 -25 | 2024 |
When a Bad Hand-rub Choice Led to an Outbreak of Candida Pelliculosa in the ICU
Vidhi Jain1*, Daisy Bacchani1, Tejashree Nare1, Vibhor Tak1, Mohan Lal1, Deepak Kumar2, Nikhil Kothari3, Ankur Sharma3
Department of Microbiology1, Department of General Medicine2, Department of Anaesthesiology & Critical Care3, AIIMS Jodhpur, Rajastha, India.
* Presenting author:– drvidhijain.micro@gmail.com
Background
The importance of hand hygiene cannot be over- emphasized. Standard alcohol-based handrubs (ABH) contain approx. 2% chlorhexidine and 60-80% alcohol. Some brands also offer emollient/ moisturizer-blended handrubs, which are softer on hands but may compromise the recommended % of constituents.
Methodology
Automated blood cultures with budding yeasts (BYCs) were identified on MALDI-TOF-MS (Biomerieux) and antifungal susceptibility was performed. A team of Microbiologists and infection control nurses conducted surveillance cultures and IPC audits, including evaluation of ABHs used in the ICU.
Result
The study was conducted from February to April 2022, when an unexpected 77 isolates of Candida pelliculosa were cultured from febrile HAI patients, susceptible to Caspofungin (84.41%), Amphotericin B (80.51%), Flucytosine (76.62%), Voriconazole (74.02%), Fluconazole (48.05%) and Micafungin (5.19%). Our investigation found the common link of all cases as the adult ICU. While surveillance cultures did not yield any Candida pelliculosa, an audit of ABHs showed a non-approved emollient ABH product with <60% alcohol being used for skin preparation, despite the availability of the standard ABH product in the store. There had been a routine shuffling of junior nursing staff between the wards and the ICU, around two months ago.
The new staff had switched to the emollient-based product for hand hygiene and had inadvertently used it for skin preparation as well. The use of the new product was immediately discontinued. A proper training was held and all the staff were re-trained. The Candida pelliculosa outbreak resolved within 10-12 days of these active interventions. Routine surveillance was strengthened.
Conclusion
We report an outbreak of Candida pelliculosa in the adult ICU of a tertiary care hospital in Western Rajasthan, which was probably caused by the use of a new inappropriate ABH product. Prompt identification, proper training and re-introduction of the appropriate ABH led to an immediate cessation of the outbreak. The use of hand rubs with unregulated constituents can compromise infection prevention and control (IPC) in the hospital.
Abstract 072 ASPICON 2024 |August 22 -25 | 2024 |
Comparison of Population Pharmacokinetics of Two Different Dosing Regimens of Vancomycin in Critically ill Patients with Sepsi
Nikhil Aravind*, Ritika Kondel Bhandari, Avaneesh Pandey, Surulivel Rajan, Sharath Kumar, Samir Malhotra, Yashwant Raj Sakaray, Neeru Sahni, Navneet Sharma, Nusrat Shafiq
PGIMER, Chandigarh, India.
* Presenting author:– nikhilaravind236@gmail.com
Background
Sepsis management requires urgent and optimized antimicrobial use. In sepsis, there is alteration of the pharmacokinetics of the drugs on account of several pathophysiological changes So, pharmacokinetic studies to optimize antimicrobial dose and improve probability of target attainment need to be conducted. Vancomycin is a key component of empiric and/or lab-based use in patients with sepsis. The aim of present study was to compare two intravenous dosing regimens 1000 mg bid and 500 mg qid in critically ill patients with sepsis and to validate nomogram generated from pop-pk-pd modeling in a sample cohort.
Methodology
The study was conducted by the Department of Pharmacology in collaboration with critical care units in a tertiary care center of North India after obtaining approval from IEC (No. INT/IEC/SPL-480) and registration with CTRI (CTRI/2023/02/049473). Eligible patients were randomly assigned to receive either the vancomycin dose routinely administered 1000 mg iv twice daily or 500 mg iv four times daily. Relevant covariate data were collected. Sparse sampling methodology with capture of trough concentrations was carried out. Structural model followed by covariate model was built using PUMAS software. Model diagnostics conducted include goodness-of-fit, visual predictive check and 1000 bootstraps to validate the model. Data simulation for 1000 mg bid and 500 mg qid were carried out for different weight and creatinine clearance combinations ranging from 45-80 kg and 50-100 ml/min. Key primary endpoint was an increased probability of target attainment.
Result
A total of 26 patients were randomized to the two treatment arms. A 2-compartment combined error model with the covariates creatinine clearance and body weight explained the data adequately. AUC0- 24/MIC estimation from simulated data showed that the number of individuals attaining the target was significantly higher in the 500 mg qid group as compared to 1000 mg bid group. Nomogram based dosing and evaluation is ongoing. The trough concentrations in the therapeutic range of 15-20 mg/L was observed for a higher proportion of patients in 500 mg qid as compared to 1000 mg bid across all creatinine clearance and weight ranges tested.
Conclusion
The results of the study indicate that a higher proportion of patients achieve the required target in 500 mg iv qid group and it may be used in therapeutics to increase clinical efficacy.
Abstract 073 ASPICON 2024 |August 22 -25 | 2024 |
Clinical Efficacy and Pharmacokinetics of Colistimethate Sodium in Critically ill Paediatric Patients Admitted in a Tertiary Care Hospital in India : A Prospective Longitudinal Observational Pilot Study
Krishnapriya N1* , Pugazhenthan Thangaraju1 , Nitin Rewaram Gaikwad1 , Atul Jindal2 , V Balasubramanian3
1-Department of Pharmacology, All India Institute of Medical Sciences, Raipur, Chhattisgarh , India.
2- Department of Pediatrics, All India Institute of Medical Sciences, Raipur, Chhattisgarh , India.
3- Raipur Amity University, Chhattisgarh, India.
* Presenting author:– priyakrishna34@gmail.com
Background
The emergence of multidrug-resistant Gram-negative infections in India’s paediatric intensive care units(PICU) has necessitated the renewed use of colistin. Current evidence on colistin’s use in Indian paediatric patients is limited, underscoring the need for further research. This study uniquely evaluates the clinical efficacy and safety of colistimethate sodium(CMS) in critically ill paediatric patients, correlating it with pharmacokinetics.
Methodology
: Children meeting the inclusion criteria were enrolled from the PICU of a tertiary care centre after obtaining parental consent. Demographic details were recorded, and blood samples were analysed for kinetic parameters using HPLC. Clinical efficacy indicators included clinical improvement or treatment failure at 72 hours, clinical cure at 14 days, all cause mortality within 28 days, ventilator days, length of PICU stay, and any adverse reactions before discharge. The microbiological outcome was culture response rate at the end of 14 days of CMS therapy. Data were managed with MS Excel (2019) and analysed using SPSS.
Result
The study included 23 patients. The main indication for colistin was sepsis (52.2%). At 72 hours, 52.2% of patients showed clinical improvement, while 47.8% had treatment failure. Clinical cure at 14 days was observed in 43.5% of patients. All-cause mortality within 28 days was 43.5%. The median PICU stay was 21 days (IQR: 13-30), and the median ventilator days were 15 (IQR: 8-21). Nephrotoxicity occurred in 6 patients (23.1%), with no cases of neurotoxicity. Culture response was observed in 61.5% of patients .Kinetic parameter results are awaited.
Conclusion
Colistin therapy, administered as loading and maintenance doses, appears to be effective and safe in the paediatric population based on clinical and microbiological outcomes.
Abstract 074 ASPICON 2024 |August 22 -25 | 2024 |
Prospective Assessment of Antimicrobial Prescribing Pattern in Medicine Intensive Care Unit of a Teaching Hospital
T Sai Pranitha*
Department of Pharmacology, Kodagu Institute of medical sciences, Madikeri, India.
*Presenting author:– pranitha8008@gmail.com
Background
Antimicrobial agents (AMAs) are one of the greatest contributions of the 20th century, used for the treatment and prevention of infections. However, their widespread use has led to the development of resistance. Understanding the pattern of their use is crucial for optimizing treatment efficacy and curbing the emergence of antibiotic-resistant organisms. Hence, it is important to evaluate the prescription pattern of AMAs to avoid irrational use of drugs.
Objectives:
1. To study the prescribing patterns of antimicrobial agents.
2.To Analyse the rational use of antimicrobial agents in the ICU
Methodology
The study was a retrospective observational study conducted over a period of three months, from January 2024 to March 2024. A total of 216 case records of patients admitted to medical intensive care unit, receiving at least one dose of antimicrobial drugs, were reviewed for the pattern and rationality of antimicrobial drug usage. Rationality was assessed by analysing adherence of antimicrobial prescriptions to Institutional Antimicrobial policy. Data were summarised and analysed using mean and percentage values.
Result
Of the total 216 patients evaluated, 65.7% were male and 34.2% were female. A common indication of AMAs use was Acute Febrile illness (AFI) at 46.3%, followed by COPD at 23.1%. The most commonly prescribed
AMAs were cephalosporins (55.56%), followed by tetracyclines (27.78%), and combination of antimicrobials from different groups (16.67 %). In 62.5% of patients, antimicrobial therapy was considered rational.
Conclusion
Prescribers did not adhere to the Institutional Antimicrobial policy in more than one – quarter of the prescriptions. This non-adherence may increase the risk of treatment failure, adverse drug reactions and the development of antibiotic resistance.
Abstract 075 ASPICON 2024 |August 22 -25 | 2024 |
Comparative Evaluation of Agar Dilution, Broth Microdilution, and Vitek-2 Methods for Detection of Colistin Resistance in Escherichia Coli Urine Isolates
Swati Nirmal*
University College of Medical Sciences is a medical college in Delhi, India
* Presenting author:– Swati.nirmal7@gmail.com
Introduction
Polymyxin (Colistin) is a novel class of antimicrobial that has a surface-active detergent-like action against most Gram-negative bacteria like Escherichia coli. The emergence of colistin-resistant bacteria, although reported infrequently to date, However, there is still no consensus regarding the breakpoints for outlining resistance to colistin.
Aim: To compare the agar dilution, broth microdilution method, and Vitek-2 for the detection of colistin resistance in E. coli urine isolates.
Materials & Methodology
A one-year cross-sectional observational study was conducted in the Department of Microbiology at Maulana Azad Medical College, New Delhi. A total of 200 E. coli isolates were subjected to Agar dilution, Broth microdilution (BMD), and Vitek-2 methods for colistin. Using BMD as the gold standard, a comparative analysis between different methods was carried out.
Result
Out of 200 E. coli isolates, Vitek-2 detected colistin resistance in six isolates. By Broth microdilution, two isolates were resistant to colistin. No isolates were resistant to colistin by the agar dilution method. Among the 198 isolates that were colistin-sensitive by the broth microdilution method, 4 were colistin-resistant by Vitek-2. All the isolates were subjected to PCR using primers targeting the mcr gene to compare the resistance pattern of colistin in E. coli isolates. Out of 200 E. coli isolates, 20 had the mcr gene.
Conclusion
The overall concordance rate was 1%, and the discordance rate was 99% between Colistin resistance from BMD and Vitek-2. Therefore, the use of molecular methods (PCR) needs to be increased for better detection of resistance marker genes in routine laboratory settings.
Abstract 076 ASPICON 2024 |August 22 -25 | 2024 |
Incidences of Missed Mucormycosis in Immunocompetent Individuals: A Study of Diagnostic Challenges and Treatment Patterns in Tbilisi, Georgia
Aastha Saurabh*
Georgian National University SEU, Tbilisi, Georgia.
* Presenting author:- aastha.saurabh2302@gmail.com
Background
Mucormycosis, typically seen in immunocompromised individuals, is a rare and diagnostically challenging fungal infection. However, recent reports suggest an increasing incidence among healthy, immunocompetent individuals. This research paper aims to highlight cases of missed mucormycosis in healthy patients, emphasizing the diagnostic challenges and efficacy of treatments post-misdiagnosis. We conducted a primary research study involving 15 respondents in Tbilisi, Georgia, and reviewed past cases of pulmonary and renal mucormycosis to understand evolving incidence patterns and diagnostic approaches. Two major hospitals in Tbilisi, where these patients were treated, were also included in the study.
Methodology
This study employed a mixed-methods approach. We conducted primary research with 15 respondents residing in Tbilisi, Georgia, to gather data on missed mucormycosis diagnoses and treatment patterns. The survey included questions about their health status, medical history, and any instances of mucormycosis diagnosis. Additionally, we reviewed case studies focusing on missed mucormycosis infections, misdiagnoses, and treatment outcomes. Diagnostic and differential diagnostic criteria were analyzed alongside novel treatment guidelines for the infection. Data from two major hospitals in Tbilisi, Georgia – Tbilisi State Medical University Clinic and Neo Hospitals – were included to provide clinical insights and case management details.
Result
Our primary research indicated that among the respondents, a significant proportion reported generalized symptoms that were initially misdiagnosed, leading to delayed treatment. Radiological findings often revealed signs indicative of mucormycosis, such as pleural effusion and multiple nodules, which were overlooked in initial assessments. The review of past cases corroborated these findings, highlighting the need for improved diagnostic criteria and awareness among healthcare providers. Both Tbilisi State Medical University Clinic and Neo Hospitals documented several cases where initial misdiagnosis led to complications, emphasizing the necessity for comprehensive diagnostic protocols.
Conclusion
Although mucormycosis presentation in healthy, immunocompetent individuals is rare, the incidence rate is increasing, necessitating vigilant differential diagnosis and prophylactic testing. Early detection and treatment initiation are crucial, as delays in such cases can prove fatal. The study underscores the importance of heightened awareness and prompt action to mitigate the risks associated with missed mucormycosis diagnosis.
Abstract 077 ASPICON 2024 |August 22 -25 | 2024 |
Diagnostic Accuracy of Point-of-Care Tests for Urinary Tract Infections: A Systematic Review and Meta-Analysis Protocol
Kusum Rani1* , Sathanarayana Reddy Bygari1, Fabia Edathadathil2 , Sanjeev Kumar Singh1
1- Amrita Vishwa Vidyapeetham, Faridabad, Haryana, India.
2- Amrita Vishwa Vidyapeetham, Kochi, Kerala, India.
* Presenting author:-sabharwalkusum24@gmail.com
Background
Urinary tract infections (UTIs) are a common health problem that leads to a considerable number of consultations and antibiotic prescriptions. The conventional diagnosis is still based on empirical methods dependent on symptoms reported by the patient and urinalysis performed using test strips, with urine culture as the gold standard despite its result turnaround of 48 hours.
Objectives: It is particularly designed to juxtapose the existing point-of-care tests for UTI in terms of diagnostic accuracy in primary and secondary care. This systematic review will help describe more effective POCTs at the point-of-care level about identification (ID) and antimicrobial susceptibility testing (AST) and their respective specificity and sensitivity.
Methods and Analysis:
This review will include studies that evaluate POCT accuracy for UTI diagnosis. Detailed literature searches in electronic databases will be conducted in PubMed, Web of Science, Embase, and the Cochrane Database of Systematic Reviews from their inception to July 2024. The studies to be included are random control trials (RCTs), cluster RCTs, observational studies, and regulatory reports reporting on direct comparisons of POCTs to standard urine culture. Data extraction will be done by two reviewers who work independently. Discrepancies will be resolved through discussion. The Quality Assessment of Diagnostic Accuracy Studies risk of bias tool, QUADAS-2, will be used to assess the
risk of bias in the studies included. A metaanalysis will be undertaken when sufficient data are available. It will use bivariate random effects models for estimating summary sensitivity and specificity, accounting for heterogeneity among studies
Ethics and Dissemination
Formal ethical approval will not be sought because no identifiable personal data will be collected. This protocol for the systematic review will be registered with PROSPERO. The findings of review will be disseminated to stakeholders, including patient groups and clinicians and also presented at conferences. This review is expected to go on and make a contribution to the understanding of the available evidence about the effectiveness of POCTs for diagnosing UTIs, which may have an impact on clinical policy.
Abstract 078 ASPICON 2024 |August 22 -25 | 2024 |
Analysis of Aetiology & Prevalence of Catheter Associated Urinary Tract Infection in a Tertiary Care Hospital of Uttarakhand
M.M. Joshi* , Garima Mittal, Arpana Singh
Department of Microbiology, Himalayan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
*Presenting author:– drmmjoshi1427@gmail.com
Background
Catheter associated urinary tract infection (CAUTI) continues to be among the most common healthcare-associated infections in India. Despite advances in prevention guidelines, there remains a lack of knowledge concerning the risk factors for CAUTI. Hence this study was undertaken for better understanding of CAUTI.
Methods
The study was conducted in a tertiary care hospital attached to a teaching institute. Retrospective analysis of CAUTI bundle data was done from March 2023 to March 2024.
Result
Out of 15,842 catheterised patients, 61 patients (0.8%) developed CAUTI. Average duration of catheterisation among CAUTI patients was 15 days. Majority of the patients belonged to the age group 40yr to 69yr, followed by above 69 yr. There was no gender disparity. Klebsiella pneumoniae (36%), Enterococcus spp (31%) & Escherichia coli (25%) were the most common pathogen identified among 61 CAUTI patients, followed by Pseudomonas aeruginosa (6.6%) and Acinetobacter baumanii complex (4.9%). Pseudomonas aeruginosa & Klebsiella pneumoniae were the most resistant pathogen among all. Total deaths among CAUTI patients were seen in 11(18%) cases probably due to MDR organisms and multiple comorbidities.
Conclusion
This study underscores the importance of a comprehensive approach to CAUTI, encompassing timely analysis, prevention & surveillance to reduce its prevalence & impact on patient care. Behavioural changes, including empowerment of nurses and adherence to all elements of the care bundle, can lead to significant and sustained improvement in reducing the CAUTI rate in hospitals.
Abstract 079 ASPICON 2024 |August 22 -25 | 2024 |
Prevalence of Aeromonas Septicemia in Cancer Patients in Tertiary Care Hospital
Virendra Kumar Jaiswar*, Sanjay Biswas, Gaurav Salunke, Shamita Binod, Anil Verma, Priyanka Singh, Jyoti Sinol
Department of Microbiology, Tata Memorial Hospital, HBNI University, Mumbai, India.
* Presenting author:– vbj13670@gmail.com
Background
Aeromonas Species (A. hydrophila, A. caviae and A. veronii) are emerging and potential human pathogens causing both intestinal and extra intestinal infections. A. hydrophila is the most prevalent Aeromonas species. It is an opportunistic pathogen and causes infections in immunosuppressed and anemic patients. The main clinical expressions are gastrointestinal tract disorders, wound, soft tissue infection and septicemia. We investigated the prevalence of Aeromonas species in cancer patients and studied their sensitivity pattern against CLSI approved antibiotics, which will help in management of clinical cases.
Methods
A 2 year retrospective study was conducted in the department of Microbiology at Tata Memorial Hospital. 179 isolates of Aeromonas species were obtained from clinical samples (blood, bile, pus, wound, urine, sputum, BAL, tracheal secretion). Identification and susceptibility testing was performed using standard guidelines by Vitek 2 system. VP Test was used to differentiate between A. hydrophilia and A. caviae.
Result
Males (59.22%) were more commonly infected with Aeromonas sp. as compared to female (40.78%) patients. Patients in the age group of 31- 65 years were most infected (76.5%). Aeromonas hydrophilia was the single most commonly isolated species. 60.9 % of the Aeromonas species were isolated from bile and PTBD followed by 17.3 % from pus/ swab and 15.7% from blood. 97.21% of the isolates were susceptible to Amikacin, followed by Gentamicin (95.53%) Imipenem (93.86%), Meropenem (92.19%), Ciprofloxacin (83.80%), Ceftazidime (80.45%), and Piperacillin-Tazobactam (51.96%).
Conclusion
Aeromonas species mainly infect the GI tract in cancer patients. Amikacin, Gentamicin, Imipenem, Meropenem shows better susceptibility towards Aeromonas species when compared with Ciprofloxacin and Ceftazidime.
Abstract 080 ASPICON 2024 |August 22 -25 | 2024 |
Microbacterium aurum Bacteremia in Immunosuppressed Patients- An Emerging Threat – Case Series
Sangram Singh Patel*, Gerlin Verghese, Nidhi Tejan, Chinmoy Sahu
Department of Microbiology, SGPGIMS, Lucknow, Uttar Pradesh, India.
* Presenting author:– sangramsgpgi@gmail.com
Background
Bloodstream infection with Microbacterium species in humans is rare and frequently linked to the presence of immunosuppressed conditions such as patients on chemotherapy or corticosteroids. Presence of indwelling catheters is also a potential risk factor for M. aurum infection. No case report has been documented in the literature regarding the pathogenic potential of M. aurum in causing bacteremia. This is the first case series reporting bacteremia by M. aurum describing the risk factors and sensitivity pattern of this pathogen. In this case series, we have described bacteremia caused by M.aurum The risk factors and sensitivity pattern of this pathogen have also been evaluated.
Cases
We have described the clinical course and presentation of three patients whose blood culture showed growth of M.aurum. Indwelling venous catheter for hemodialysis or for chemotherapy for the treatment of acute lymphoblastic leukemia was found to be a risk factor in two patients. Rheumatoid arthritis was the underlying condition in the second patient and was started on immunosuppressants. Blood samples were collected during the febrile period. The blood culture samples of all these patients had pure isolates of M. aurum, identified by matrix-assisted laser desorption ionization–time of flight mass spectrometry. All three isolates were susceptible to ceftazidime and doxycycline. The patients were managed according to the sensitivity reports and were discharged in stable condition.
Conclusion
Microbacterium aurum can cause bacteremia in immunocompromised patients but respond well to susceptibility guided antibiotic therapy.
Abstract 081 ASPICON 2024 |August 22 -25 | 2024 |
Unravelling the Trends of Sexually Transmitted Infective Syndromes Reported in an Apex Regional Centre
Pragyan Swagatika Panda1* , Abhishek Lachyan2 , Sumathi Muralidhar3
1-Department of Microbiology, VMMC and Safdarjung Hospital, New Delhi-29
2-Department of Obstetrics and Gynaecology, VMMC and Safdarjung Hospital, New Delhi-29
3- Apex Regional STI Centre, Safdarjung Hospital, New Delhi-29
* Presenting author:– pragyanpanda2006@gmail.com
Background
Sexually transmitted infections (STIs) pose a significant global public health challenge. The significance of addressing STI syndromes cannot be overstated. Publicly, they contribute significantly to the global disease burden, necessitating targeted interventions. Timely identification and treatment are pivotal at an individual level, preventing complications and enhancing overall health. Managing STI syndromes also aids in preventing transmission within communities and mitigating threats of antibiotic resistance. This study examines the demographic profiles of STI healthcare seekers, focusing on GUD Herpetic, Non-Herpetic, Vaginal, Cervical, and urethral discharge syndromes and analyses monthly trends to contribute insights for adaptive public health strategies.
Methods
A retrospective analysis of patient records from July 2022 to June 2023 was conducted. Demographic data, syndrome classification, and monthly trends were systematically extracted and analysed.
Results
The demographic analysis revealed distinct gender patterns among individuals seeking STIrelated healthcare. Males were predominant in GUD Non-Herpetic (87.88%) and GUD Herpetic syndromes (66.89%), while females dominated VDRL testing, comprising 79.14% of cases. Syndromic classification further highlighted variations, emphasizing the importance of gender-specific factors in STI dynamics.
Monthly trend analysis depicted the dynamic nature of STIs, with fluctuations in reported cases. GUD non-herpetic syndrome peaked in April 2023 (6 cases), while GUD Herpetic and vaginal discharge peaked in December 2022 (19 and 96 cases respectively), indicating diverse seasonal trends in different syndromes. Amongst the GUD non-herpetic cases Syphilis was more common compared to Chancroid and Donovanosis.
Conclusion
This study provides significant insights into STI epidemiology, demographic profiles, syndrome prevalence, and temporal trends. Continuous monitoring and adaptive public health measures are crucial for addressing emerging patterns. Acknowledging limitations, prospective studies on socio-cultural factors’ impact on STI dynamics are warranted.
Abstract 082 ASPICON 2024 |August 22 -25 | 2024 |
Seroprevalence of Leptospirosis in a Tertiary Care Hospital in Mumbai, India
Tejasvini Sonavane*, Jyoti Bala, Nupur Chandra, Meghna Palwar, Nilma Hirani
Department of Microbiology GGMC, Mumbai, Maharashtra, India.
* Presenting author:– tejasvonisonvane@gmail.com
Background
Leptospirosis, a widespread re-emerging zoonotic disease especially in developing countries like India. According to WHO more than 5 lakh cases of leptospirosis are reported worldwide per year with mortality more than equal to 10% and its outbreak has been increased for the past 3 decades.
Aim: This study aims to determine the seroprevalence of leptospirosis among febrile patients at tertiary care hospital Mumbai.
Methods
It is a retrospective observational laboratory-based study over a period of one year in tertiary care hospital, Mumbai. A total of 5566 blood samples of febrile patients received for diagnosis of leptospirosis IgM antibodies using ELISA.
Results
A total of 1173 of 5566 blood samples that were received during the study period tested positive for leptospirosis IgM antibody. Seroprevalence of leptospirosis was found to be 21.07 % with maximum incidence observed during monsoon.
Conclusion
Leptospirosis has emerged as a health challenge among patients with acute febrile illness especially during monsoon, hence early diagnosis & proper antibiotic treatment is necessary to decrease mortality and morbidity.
Abstract 083 ASPICON 2024 |August 22 -25 | 2024 |
Factors Influencing Patient Adherence to Prescribed Antifungals in Dermatophytosis and its Impact on Treatment Outcomes
Nidhi Sharma*
Department of Dermatology, Government Medical college, Jammu, India.
* Presenting author:– Needee88@gmail.com
Background
Adherence to treatment protocol is of paramount importance in all areas of clinical medicine, including dermatology. Unfortunately, various reports in literature suggest that adherence may be the exception rather than the rule. There has been an unprecedented epidemic-like scenario of dermatophytosis in India in the past few years and nonadherence to treatment protocol is postulated as one of the most important factors contributing to it. This study aimed to investigate the factors that contribute to patient adherence to prescribed antifungal medications in treatment of dermatophytosis and examines how adherence influences treatment outcomes.
Methods
This was a cross-sectional descriptive study carried out over a period of one year in which clinically diagnosed patients of tinea infection were enrolled. The study employed a mixed-methods approach, combining quantitative surveys regarding demographic information, followed by clinical examination regarding type of dermatophyte infection; and qualitative interviews regarding understanding of treatment, medication-related beliefs, socioeconomic factors and other perceived barriers to adherence, to comprehensively explore the factors influencing patient adherence to prescribed antifungal medications. Finally the treatment outcomes in terms of mean duration of therapy for disease control and side effects were observed and compared
Results
A total of 500 patients, comprising 233 men and 267 women aged 18-60 years were included in the study. Tinea corporis was the most common variant seen in 260 (52%) patients followed by Tinea cruris (31.6%), Tinea faciei (7%), Tinea pedis (5.2%), Tinea mannum (3.4%) and Tinea barbae (0.8%). Only 8.8% of patients were treatment naïve with the majority of the patients having taken topical or oral antifungal treatment in the past. Antifungals were prescribed by dermatologists in 19.5% cases, general practitioner (GP) in 27.4% cases, local chemist (38.1%) and self-medication by 14.9% patients through TV advertisements.
Majority of the patients treated by GP, local chemist and self-medication; used topical steroid containing cream (92.6%) and oral fluconazole (56%). While itraconazole (88.2%) and topical luliconazole (78.6%) was most commonly prescribed by dermatologists. Factors affecting adherence were poor instructions given to patient by prescriber (34.2%), cost issues (29.3%), patients belief regarding safety of medication (17.8%), lack of patient education regarding disease (10.7%), poor memory on part of patients (7%) and side effects (3%).The average duration of antifungals treatment in the non-adherence group was 13.4 weeks.
Conclusion
These findings will provide valuable insights into the existing knowledge gaps and aid in designing targeted educational programs and interventions to enhance treatment adherence which might improve treatment outcomes.
Note: Few presented abstracts were removed in this publication considering lack of data or incompleteness. |
Abstract Author Index
The number(s) following each author’s name indicate the corresponding abstract number.
A.N. Aggarwal; 15 Aastha Saurabh; 76 Abdul Asma mohe; 52 Abhishek Lachyan; 81 Adarsh Patil; 69 Adithya Lingala; 69 Ajay Halder; 12 Amandeep Gondara; 37 Amit Arora; 32 Amit Kumar Mathur; 04 Amrutha T.S; 25 Ananya Arora; 02, 58 Anil Kumar; 34 Anil Verma; 79 Anisha Yadav; 39 Anjleen Kaur; 53 Ankur Goyal; 44, 65 Ankur Sharma; 71 Ankush Goyal; 19 Anu Nosran; 34 Anupam Berwa; 54 Anuradha Chaudhary; 38 Anuradha Gandhi; 10 Anuradha Mishra; 05 Anuradha Sood; 38 Anwita Mishra; 48 Aparna Chakravarty; 68 Archana; 64 Archana Angrup; 32, 61 Arpana Singh; 78 Arpita Panda; 33 Arti Agarwal; 44 Arti Agrawal; 64, 65 Arunima Sehgal Mukherjee; 34, 35 Asheema Khosla; 70 Ashima Katyal; 39 Asim Kumar Kundu; 59 Atul Jindal; 73 Avaneesh Pandey; 72 Avinash Turankar; 46 Ayana Jain; 14 Ayekpam Minerva; 20 Balvinder Mohan; 18, 26 Barasha Das; 64 Barnali Kakati; 40 Basira Sultan; 49 Benu Dhawan; 51 Bhatia NJK; 47 Bhawna Sharma; 41 Bhupinder Solanki; 16 Bimal Kumar Das; 51 Chaudhary Anuradha; 30 Cherring Tandup; 32 Chetan Chandel; 09 Chetana Nandaniya; 50 Chetna Desai; 10 Chinmoy Sahu; 22, 80 Chirag Modi; 50
Choudhary Anuradha; 03 Daisy Bacchani; 71 Darab Singh; 04 Debasish Biswal; 02, 51, 66 Deepa Devhare; 14 Deepak Kumar; 71 Deepinder Singh; 39 Devraj Dogra; 49 Dharmendra Singh; 18 Dhulika Dhingr; 58 Dipti Pattanaik; 31 Divya Darshan Panigrahi; 08 Divya Nair; 32 Ekta Rawat; 65 Fabia Edathadathil; 77 Farhan-ul-Huda; 16 Garima Mittal; 78 Gaurav Salunke; 25, 56, 79 Gerlin Verghese; 22, 80 Gulam Gouse; 16 Guru Mehar Sharma; 27 Harpreet Kaur; 18, 26 Harpreet Singh; 37 Harshil Damor; 10 Hemangi Kadlak; 29 Hitender Gautam; 51 Intezaar Ahmed; 16 Ipsa Mohapatra; 31 Isampreet Kaur; 38 Ishan Verma; 69 Jaideep Pilania; 43 Jasbir Singh; 19, 23, 53 Jasmeen; 19, 24 Jyoti Bala; 67, 82 Jyoti Chaudhary; 60 Jyoti Choudhary; 01 Jyoti Sangwan; 21 Jyoti Sinol; 56, 79 K. Pushpalatha; 12 Kalpana Mund; 31 Kalyan Samanta; 11 Kanchan Dochania; 15
| Kanugula Harika; 52 Kashyap Saleena; 30 Kaur Isampreet; 03, 30 Khushboo Bisht; 66 Krishnapriya N; 73 Kritika Milind Dongre; 46 Kusum Rani; 77
Lily Dubey; 27, 36 M.M. Joshi; 78 Mahadevan Kumar; 14 Maitrayee Narayan; 51 Mallika Nanda; 35 Mamta Senger; 42 Manisha Aggarwal; 01, 60 Manisha Subarao Mane; 13, 28 Mansi Gupta; 08 Marapalli Sindhoora; 28 Meenakshi Chakraborty; 68 Meenalotchini P Gurunthalingam; 06 Meghna Palawer; 67, 82 Menal Gupta; 60 Minakshi Dhar; 66 Mohan Lal; 71 Mukesh Bairwa; 04 M. Z. Abdin; 05 Naimika Patel; 50 Narinder Kaur; 07 Naveen Chaudhary; 18, 26 Naveet Wig; 51 Navjot Kaur; 19, 23, 24, 53 Navneet Sharma; 72 Neelam Taneja; 18, 26, 34, 37, 61 Neeru Sahni; 72 Neetu Sharma; 24 Neha Joshi; 45 Nitika Rana; 32 Nidhi Sharma; 49, 83 Nidhi Tejan; 22, 80 Nikhil Aravind; 72 Nikhil Kothari; 71 Nikunj R. Agrawal; 57 Nilanjana; 04 Nilesh Kamble; 69 Nilma Hirani; 67, 82 Nipa Singh; 31 Nithin Varghese; 08 Nitin Gaikwad; 06 Nitin Rewaram Gaikwad; 57, 73 Nitish Sharma; 55 Nupur Chandra; 67, 82 Nupur Koul; 40 Nusrat Shafiq; 34, 37, 72 Oshin Sinha; 35 P. L Gautum; 01 Pallab Ray; 32 Pandey P; 47 Poonam Arora; 62 Pradnya Samant; 25 Pragya Shakya; 44, 64, 65 Pragyan Swagatika Panda; 33, 81 Prasan Kumar Panda; 04, 43, 66 Prashant Parmar; 27 Pratibha Kale; 63
Pratibha Mane; 21 Pratip Das; 06 Preety Mishra; 31 Prerna Aggarwal; 39, 54 Prerna Khurana; 42 Prity Gupta; 48 Priyal Gupta; 12 Priyanka Singh; 08, 79 Pugazhenthan Thangaraju; 73 Puneet Dhamija; 16 Puneet Kaur; 19, 24, 53 PVR Narendra Babu; 27 Rahul Sarode; 48 Rai B; 47 Raj Kishore Sahu; 29 Raja Chakraverty; 11, 59 Rajesh Kumar Dash; 31 Rajesh Mahajan; 01 Rajesh Rana; 15 Rajni Sharma; 20 Rakesh Yadav; 15 Rakhi Maiwall; 63 Rama Gupta; 60 Raman Chauhan; 35 Ramya Rajendran; 13 Ranjana; 19 Rashi Banta; 45 Rashmi Suria; 35 Rashmi Surial; 09, 37 Ravi Kant; 04, 16 Ravi Kumar Maurya; 18 Richa Kansal; 39 Rishiraj Bhatt; 63 Ritika Kondel Bhandari; 34, 72 Rohit Garg; 02 Rohit Gupta; 16 Rungmei S K Marak; 22 Rupal Patel; 50
| S.K. Singh; 20 Sachin Kumar Sharma; 62 Sadia Khan; 68 Sahil Kumar; 35 Samir Malhotra; 72 Sandeep Kaushal; 01 Sangram Singh Patel; 22, 80 Sanjay Biswas; 56, 79 Sanjeev Kumar Singh; 66, 77 Santhosh Harkal; 25 Santosh Harkal; 56 Sarita Mohapatra; 51 Sarita Sherawat; 21 Sathanarayana Reddy Bygari; 77 Seema Sood; 51 Shahbaz Aman; 07 Shailza Balu; 23 Shalini Mandal; 23 Shalini Mann; 08 Shamita Binod; 79 Sharath Kumar; 72 Shariqa Qureshi; 42, 58 Sharma Manvi; 30 Sharmila Sengupta; 02, 68 Shashank Purwar; 12 Shashank Tiwari; 48 Shashi Marko; 27, 36 Shazia Hasan; 16 Shikhar Saxena; 17 Shraddha Paralkar; 14 Shubhangi Kansal; 61 Shulania A; 47 Shweta Singhal; 44 Singh Gargi; 03 Sivasakthi C; 46 Sonali Bhattar; 17 Sood Anuradha; 03, 30 Soumya Nayak; 31 Subhash Chand; 45 Subhra Snigdha Panda; 31 Sujit Bharti; 48 Sukant Pandit; 46 Sumathi Muralidhar; 81 Sundeep Sahay; 34, 35 Sunil Dhatwalia; 15 Sunil Kumar Raina; 35 Sunil Sethi; 15 Sunita Kumbhalkar; 69 Surulivel Rajan; 72 Swathi Suravaram; 52 Swati Nirmal; 75 Syeda Saba Hashmiya; 13, 28 T Sai Pranitha; 74 Tanvi Vashist; 32 Tanya Arora; 40 Tejashree Nare; 71 Tejasvini Sonavane; 67, 82 Tulika Choudhary; 17 Tushar Chauhan; 53 U. Soniya Soundari; 54 Ujjwala Gaikwad; 08 V Balasubramanian; 73 Veena Balothia; 20 Veenu Gupta; 01, 60 Vibhor Tak; 71 Vidhi Jain; 71 Vijeta Bajpai; 48 Vikas Dogra; 17 Vikas Khillan; 63 Vikas Sharma; 32 Vikash Kumar Bhati; 36 Vinay Modgil; 18, 26, 35, 37, 38 Vipasha; 07 Virendra Kumar Jaiswar; 79 Vishal Mishra; 10 Vivek Karol; 37 Vrushali Thakar; 14 VS Pai; 04 Yashwant Raj Sakaray; 72 Yogendra N. Kec; 57 |
Submit a Manuscript:
Copyright © Author(s) 2024. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

