Sepsis - Definition and Classification in Indian Setting: An Update
JASPI March 2025 / Volume 3 /Issue 1
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Pilania J, Panda PK.Sepsis – Definition and Classification in Indian Setting: An Update. JASPI. 2025;3(1):1-3 DOI: 10.62541/jaspi073
INTRODUCTION
Sepsis is a critical global health concern, claiming millions of lives annually and placing a significant burden on healthcare systems worldwide. Despite advancements in medical science, diagnosing and managing sepsis remains challenging, particularly in resource-limited settings. Recognized as a global health priority by the World Health Organization (WHO) in 2017, sepsis demands urgent attention and innovative approaches to improve patient outcomes.1
The origin of the term sepsis dates to more than 2700 years ago when the Greek word “sepo” was used by the physician Hippocrates, meaning “I rot”, for description of a process of internal decay, believed to happen to unlucky individuals.2 Over time, its understanding and definition has changed to its latest definition, as “life-threatening organ dysfunction caused by a dysregulated host response to infection”, as per the latest surviving sepsis campaign: International guidelines for management of sepsis and septic shock, 2021 (Sepsis-3).3
In 1992, convention of experts formalized the universal definition of sepsis, and it was identified as “an inflammatory process triggered by infection” , and was clinically diagnosed based on the presence of two or more signs of SIRS together with evidence or suspicion of an infection.4,5 This was widely utilized for more than two decades despite facing criticism, the major one being that the SIRS criteria frequently reflected an appropriate physiological response to infection rather than indicating a pathological condition The SIRS criteria—including fever, tachycardia, hypotension, and leukocytosis—highlight the inflammatory response, a hallmark of various critical conditions such as trauma, pancreatitis, and postsurgical inflammation 6
Because inflammation is a natural and often beneficial response to infection, defining sepsis presents the challenge of differentiating between a normal immune reaction and the severe, dysregulated inflammatory response seen in life-threatening sepsis 7
The 2016 Sepsis Task Force defined sepsis as a life-threatening state of organ dysfunction triggered by a dysregulated response of the host to infection 3 Clinically, sepsis is identified by an acute rise of two or more points in the SOFA score in the context of suspected infection 3,8 There are various available scoring systems such as SOFA, NEWS, APACHE, LODS, etc., which predict the prognosis in terms of morbidity and mortality related to sepsis, however, they can’t diagnose sepsis with accuracy. More than 250 biomarkers have been identified and studied in the context of sepsis, but only procalcitonin (PCT) and c-reactive protein (CRP) have some use. None of the biomarkers lack the sensitivity and specificity for the diagnosis of sepsis.
As part of broader antimicrobial stewardship efforts, sepsis definition and/or its classification for the right diagnosis enables the rational use of antimicrobials, thus playing a significant role in combating antimicrobial resistance (AMR), especially by reducing the misuse of antimicrobials. However, the whole world is looking for it, especially in terms of classification, including India.
SEPSIS UPDATE FROM INDIAN SETTING
Due to these shortcomings in the latest definition/classification of sepsis and the absence of any gold standard test to diagnose sepsis, a recent longitudinal observational study was conducted at All India Institute of Medical Sciences (AIIMS) Rishikesh, a tertiary care and teaching centre in the North of India, spanning over 12 months.9 This study formulated and utilized a new three-step method developed for classifying sepsis, whose flowchart and other details are depicted in Figure 1 and Table 1. NEWS-2 score, being relatively much easier to use with parameters not requiring laboratory investigations, was used to find evidence of dysregulated host response, however, no specific modifications or adaptations were done, used in its original form, for this study.
Figure 1: 3-Step Model for sepsis classification.
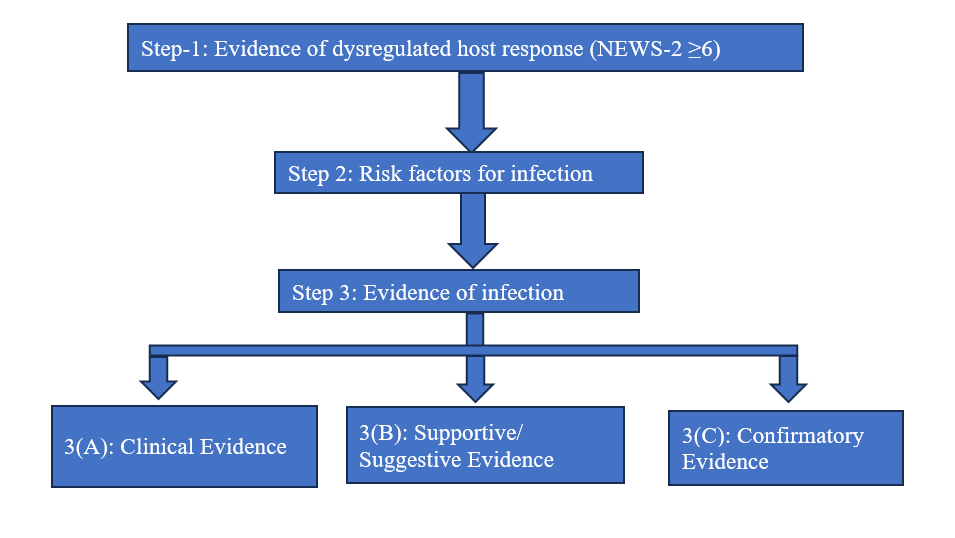
Table 1: Proposed criteria for Sepsis Classification.
Steps | Description | ||||||||||
Step 1: Evidence of Dysregulated Host Response | Assessed using the National Early Warning Score-2 (NEWS-2) ≥6 | ||||||||||
Step 2: Risk Factors for Infection | Evaluated based on the presence of risk factors such as chronic illnesses, malnutrition, unhygienic living conditions, immunosuppressive states, age, trauma, structural diseases, recent surgery, travel history, animal bites, and previous hospitalizations | ||||||||||
Step 3: Evidence of Infection | Determined through: | ||||||||||
3(A) Clinical Evidence | Syndromic diagnosis including pyelonephritis, infective endocarditis, intra-abdominal infections, skin and soft tissue infections, meningitis, cerebrospinal fluid shunt infections, catheter-related infections, osteomyelitis, abscesses, and pneumonia | ||||||||||
3(B) Supportive/ Suggestive Evidence | Imaging (X-ray, ultrasound, computed tomography, magnetic resonance imaging, positron emission tomography) and biomarkers (blood, urine, other fluids) | ||||||||||
3(C) Confirmatory Evidence | Direct visualization, endoscopic evidence, microscopy and culture growth, polymerase chain reaction/gene detection, and immunological methods | ||||||||||
Proposed criteria to classify sepsis:
| |||||||||||
This study included 230 patients as per inclusion criteria from screened 1867 patients who were on antimicrobials and were categorized into various sepsis categories (asepsis, possible, probable, and confirmed sepsis as per model) on various days during hospital stay (Day-1, 7, 14 and outcome) demonstrating the dynamic nature of sepsis. The study showed a significant finding that throughout the hospital stay, the sepsis category was changed from the initial majority of the probable sepsis group to the final majority of the asepsis group; similar trends were also observed in other groups.
One of the most significant findings from this study is that one can classify sepsis into asepsis, possible, probable, and confirmed sepsis from day zero of admission into the hospital based on available evidence, and with time, it can reclassify the same as evidence emerges. Many scoring and classification systems, simple and complex, are available for sepsis globally; however, they do not incorporate any aspects of sepsis for diagnosis, such as risk factors, clinical scenarios, and the dynamic nature of sepsis, making their use limited for sepsis diagnosis, therefore, used for majorly for prognostication and mortality assessment.10 Hence, they are not true sepsis classification systems. The various available scores for sepsis are majorly of prognostic significance rather than providing primary diagnostic importance, and this lacuna can be fulfilled with the utilization of this 3-step novel approach, which primarily focuses on the diagnostic part of sepsis followed by its management strategies. Deaths due to AMR is rising and will rise further to devasting levels if not controlled, as recently predicted in a global database.11 This is the right time to classify sepsis first; then, only data on AMR mortality in sepsis can be predicted correctly.
CONCLUSIONS
This study explores challenges in sepsis diagnosis and ways to overcome them, emphasizing a structured approach, particularly in the resource-limiting settings. The three-step approach, when integrated with the NEWS-2 score, provides a useful and pragmatic framework for early and accurate identification. It highlights sepsis classification as a dynamic process, calling for further research to refine diagnostic criteria and develop tools to distinguish sepsis from similar conditions. Enhancing the early detection of sepsis can greatly decrease morbidity and mortality, supporting the WHO’s global health objectives . The 3-step model effectively classifies sepsis into asepsis, possible, probable, and confirmed cases. Multi-centric validation studies can confirm its accuracy, with organisations like SASPI potentially leading India in this effort. With careful implementation, this approach could transform sepsis management in resource-limited settings, reducing antimicrobial misuse and combating AMR.
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
REFERENCES
Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing Sepsis as a Global Health Priority – A WHO Resolution. N Engl J Med. 2017 Aug 3;377(5):414-417. https://doi.org/10.1056/NEJMp1707170
Ackerman MH, Ahrens T, Kelly J, Pontillo A. Sepsis. Critical Care Nursing Clinics. 2021 Dec1;33(4):407-18; https://doi.org/10.1016/j.cnc.2021.08.003
Singer M, Deutschman CS, Seymour CW et al. The Third Inter- national Consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801-810 https://doi.org/10.1001/jama.2016.0287
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992; https://doi. org/10.1097/00003246-19920600000025
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101(6):1644-55 https://doi.org/10.1378/chest.101.6.1644
Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, et al. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence In Acutely Ill Patients (SOAP) study. Intensive care medicine. 2006 Mar;32:421-7. https://doi.org/10.1007/s00134-005-0039-8
Font MD, Thyagarajan B, Khanna AK. Sepsis and Septic Shock-Basics of diagnosis, pathophysiology and clinical decision making. Medical Clinics. 2020 Jul 1;104(4):573-85. https://doi.org/10.1016/j.mcna.2020.02.011
Abraham E. New Definitions for Sepsis and Septic Shock: Continuing Evolution but With Much Still to Be Done. JAMA. 2016 Feb 23;315(8):757-9. https://doi.org/10.1001/jama.2016.0290
Pilania J, Das A, Panda PK, Chauhan U. 3-step Model-An Explorative Novel Approach to Classify Sepsis: A Longitudinal Study. JASPI.2024;2(3):-15-21 https://doi.org/10.62541/jaspi046
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-247.https://doi.org/10.1007/s00134-021-06506-y
GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet. Published online September 13, 2024; https://doi.org/10.1016/S0140-6736(24)01867-1
Submit a Manuscript:
Copyright © Author(s) 2025. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

