An Unusual Case of Schistosomiasis Mimicking Colon Malignancy: Diagnostic Conundrum
JASPI June 2025 / Volume 3/Issue 2
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Mahapatra P, Kar P, Mohapatra A, et al.An Unusual Case of Schistosomiasis Mimicking Colon Malignancy: Diagnostic Corundum. JASPI. 2025;3(2): 30-33 DOI: 10.62541/jaspi078
ABSTRACT
Schistosomiasis remains a rare and underdiagnosed trematode parasitic infection in the Indian subcontinent. We present a case of a 52-year-old diabetic patient, suspected to have colonic cancer with altered bowel habits and occasional rectal bleeding symptoms. Radiological findings of contrast-enhanced computed tomography(CECT) suggested colonic malignancy, while all other malignancy workups were negative. Colonoscopic biopsy findings revealed non-specific colitis, indicating high suspicion towards parasitic foci. Few Schistosoma mansoni ova were found after direct stool microscopy, leading to[PP1] the diagnosis of Schistosomiasis. The patient was treated with albendazole along with praziquantel and showed marked clinical improvement. Radiologically, intestinal schistosomiasis may resemble other gastrointestinal disorders, like colonic neoplasms. This case highlights the need for clinicians and microbiologists to maintain a high index of suspicion for schistosomiasis in patients exhibiting colonic lesions, aided by accurate microbiological tests such as stool microscopy, particularly in underdiagnosed areas.
KEYWORDS: Schistosoma mansoni, Stool microscopy, Praziquantel, Biopsy, Colon Malignancy
BACKGROUND
Schistosomiasis, an infectious disease caused by trematode flatworms belonging to the genus Schistosoma, continues to pose a considerable public health challenge in regions where it is endemic or underdiagnosed.1 While it predominantly impacts the urinary and gastrointestinal systems, its chronic manifestations may simulate suspicion for neoplasms.2 Colonic schistosomiasis, although relatively infrequent, can present with nonspecific clinical manifestations such as abdominal discomfort, unusual bowel patterns, rectal haemorrhage, or lymphatic enlargements. These clinical presentations can closely resemble those of colonic carcinoma, thereby creating a diagnostic dilemma.3
Here, we would like to discuss an unusual case in which a Schistosoma infestation was identified incidentally during the assessment for a suspected colonic neoplasm.
CASE PRESENTATION
A 52-year-old diabetic male presented to our emergency unit with complaints of intermittent lower abdominal pain, altered bowel habits (frequent loose stool), and occasional rectal bleeding over the past 2 months. It was associated with significant weight loss, although no travel history was recorded. Physical examination was normal except for mild tenderness in the left lower quadrant.
Routine blood investigations were within normal limits except for microcytic hypochromic anaemia (Hb:10.5 gm/dl) and mild eosinophilia(365cells/ml; AEC normal range: 30- 350 cells/ml)[PP1]. Ultrasonography of the abdomen was normal, but upper gastrointestinal endoscopy suggested antral gastritis. Simultaneously, anileocecal colonoscopy revealed three columns of grade II internal haemorrhoids at the 3,7 &11 O’clock positions of the upper anal canaland a biopsy was taken. The CECT of the abdomen and pelvis showed[PP2] subtle fat stranding with inflammation& thickening around the ileum and sigmoid colon, few subcentric mesenteric nodes along the proximal mesentery, peripancreatic, precaval, periportal, left gastric artery, paraaortic, and aortocaval nodes, further raising the suspicion of [PP3] colon malignancy. A routine stool examination was sent, and it revealed structures resembling Schistosomamansoniova with lateral spinal surrounding occasional fat globules and red blood cells (Figure 1). The modified ZN stain of the stool was negative.
Figure 1. Schistosoma mansoni ova showing the typical lateral spine in direct stool wet mount microscopy (40X)
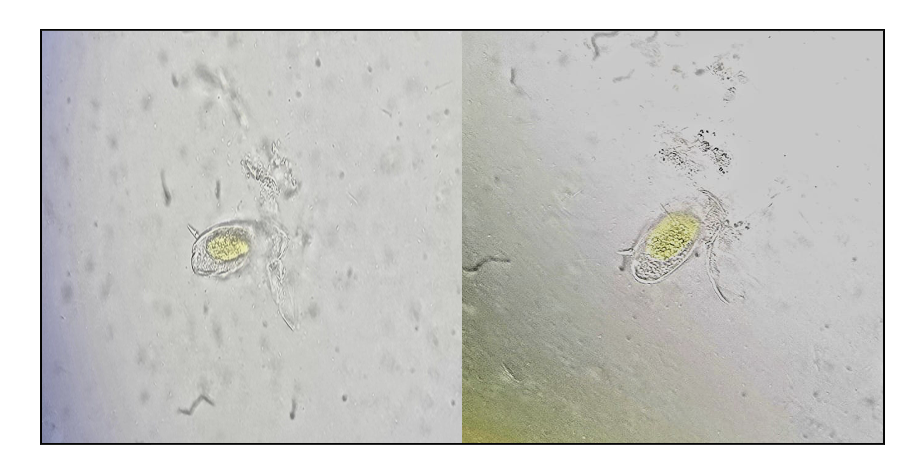
Ileum biopsy revealed non-specific colitis, which can be suggestive of parasitic infection. A [PP4] diagnosis of colonic schistosomiasis (infected by Schistosoma mansoni) was made based on stool microscopy (Figure 1), thus ruling out the malignancy. The patient was treated with albendazole (20mg/kg twice given; 1.2gm two doses for 2 consecutive days) along with praziquantel [PP5] (40mg/kg; in this case, 2.4gm given once) and showed marked clinical improvement on follow-up.
DISCUSSION
Schistosomiasis is a chronic parasitic disease, both endemic and underdiagnosed in parts of Africa, South America, the Middle East, and Southeast Asia.1 The intestinal form, mostly caused by Schistosoma mansoni or S. japonicum, can involve the colon and rectum, leading to a wide variety of clinical presentations. While many cases remain asymptomatic or present with mild gastrointestinal symptoms like colitis & abdominal pain, chronic infection can result in granulomatous inflammation, ulceration, pseudo polyps, and even strictures in the bowel wall. In rare instances, as illustrated in this case, schistosomal lesions can mimic colorectal malignancy both endoscopically and radiologically[PP1]. Similar findings of multiple lymphadenopathy and colonic inflammation in CECT abdomen and pelvis were reported by Alyhari et al.(2022)4 and Alzahran et al.(2019)5, respectively, which were suggestive of malignant aetiology. Our study revealed non-specific chronic colitis in the ileum biopsy, which was suggestive of parasitic aetiology. Alzaharani et al. (2019) revealed chronic inactive colitis, mild crypt distortion, with no dysplasia or malignancy signs in colonoscopic sigmoid colon biopsy, pointing towards other aetiologies5. This overlap can lead to diagnostic confusion or unnecessary surgical interventions if parasitic infection is not considered as one of the differential diagnoses, particularly in endemic zones and previously exposed individuals.6
The stool microscopy remains the gold standard, revealing characteristic Schistosoma ova surrounded by red blood cells. Stool microscopy, specifically the Kato-Katz methodology, has historically been regarded as the benchmark for the diagnosis of intestinal schistosomiasis owing to its good specificity in identifying the distinctive ova structure of Schistosoma. This technique facilitates the assessment of both the prevalence and the intensity of infection, leading to better epidemiological investigations and intervention strategies.6 Early diagnosis followed by appropriate management is crucial, as treatment with antiparasitic agents such as praziquantel is highly effective in approximately 60-90 % of cases7 and can prevent further complications like fibrosis and portal hypertension.8 However, recent studies have emphasised the limitations of stool microscopy sensitivity, especially in low-load parasitic infections. For instance, a study evaluating various diagnostic tests found that while microscopy is highly specific, its sensitivity is lower in cases with low parasite loads, potentially leading to underdiagnosis in areas with declining transmission rates.9 To address these above challenges, alternative diagnostic modalities like circulating cathodic antigen (CCA) tests and polymerase chain reaction (PCR) assays have demonstrated higher sensitivity in detecting low parasitic load infections.6,10 In our case, we were unable to perform these tests as they were costly and advanced parasitic diagnostic modalities were not widely available in our region.
Despite these advancements, microscopy remains a cornerstone in schistosomiasis diagnosis due to its cost-effectiveness and ability to provide quantitative data on the parasiticload.11 This case lays emphasis onthe need for clinicians and microbiologiststo have a high suspicion ofschistosomiasis in patients presenting with colonic lesions,especially in endemic or underdiagnosed areas. Awareness of this potential mimicry is essential to avoid misdiagnosis and to ensure appropriate management.
CONCLUSIONS
This case highlights the diagnosis of schistosomiasis mimicking colonic cancer. Clinicians should consider suspicion of schistosomiasis in patients with chronic gastrointestinal clinical manifestations. Early detection via simple microbiological workup like direct stool microscopy can avert unnecessary procedures and facilitate prompt specific antiparasitic therapy. This case emphasises the need for thorough clinical assessment and contextually informed diagnostics to differentiate parasitic infections from neoplasms.
ACKNOWLEDGEMENT:
We would like to express our sincere gratitude and heartfelt appreciation to Prof. (Dr.) Rajashree Panigrahy, Laboratory Director (Central laboratory) and Prof. (Dr.) Kundan Kumar Sahu, HOD, Department of Microbiology of IMS and SUM Hospital, Bhubaneswar, for providing all facilities regarding the study.
ETHICAL STATEMENT
Ethical approval was not required for this case report as per institutional policy, since it involved a single clinical observation with no experimental intervention. Written informed consent for publication of the clinical details was obtained from the patient (or their legal guardian). All identifying information has been anonymised in accordance with the Declaration of Helsinki and CARE guidelines.
CONFLICT OF INTERESTS STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None.
AUTHOR’S CONTRIBUTIONS
PM: Conceptualization; Data curation; Analysis; Writing the draft
PK: Investigation; Methodology; Resources, Review & editing
AM: Supervision, Validation, Review & editing.
RD: Conceptualization, Methodology, Validation, Review & editing
SK : Analysis, Supervision, Validation, Review & editing
DECLARATION FOR THE USE OF GENERATIVE ARTIFICIAL INTELLIGENCE (AI) IN SCIENTIFIC WRITING:
None
REFERENCES
World Health Organization. Schistosomiasis. [Internet]. 2024 [cited 2025 May 4]. Available from: https://www.who.int/news-room/fact-sheets/detail/schistosomiasis
Chitsulo L, Engels D, Montresor A, Savioli L. The global status of schistosomiasis and its control. Acta Trop. 2000;77(1):41–51. doi:10.1016/S0001-706X(00)00122-4
Gray DJ, Ross AG, Li YS, McManus DP. Diagnosis and management of schistosomiasis. BMJ. 2011;342:d2651. doi:10.1136/bmj.d2651
Alyhari Q, Ahmed F, Al_Shaibani H, Al_Kubati M, Alhadi A. Huge colonic granuloma of schistosomiasis mimicked cancer in a 10-years-old child: a case report. International Medical Case Reports Journal. 2022 Dec 31:379-84.
Alzahrani AR, Alawfi H, Almeman S, Altayeb T, Al-Dorzi HM. Megacolon due to chronic schistosomiasis: a case report and review of literature. Case Reports in Surgery. 2019;2019(1):4036823.
Ally O, Kanoi BN, Kamath S, Shiluli C, Ndombi EM, Odiere M, Misinzo G, Nyanjom SG, Kumar CK, Ochola L, Lolabattu SR. Development of a rapid and highly sensitive nucleic acid-based diagnostic test for schistosomes, leveraging on identical multi-repeat sequences. Frontiers in Parasitology. 2024 Mar 14; 3:1361493.
Hechenbleikner EM, McQuade JA. Parasitic colitis. Clinics in colon and rectal surgery. 2015 Jun;28(02):079-86.
Kali A. Schistosome infections: an Indian perspective. Journal of clinical and diagnostic research: JCDR. 2015 Feb 1;9(2):DE01.
Ally O, Kanoi BN, Ochola L, Nyanjom SG, Shiluli C, Misinzo G, Gitaka J. Schistosomiasis diagnosis: Challenges and opportunities for elimination. PLOS Neglected Tropical Diseases. 2024 Jul 11;18(7):e0012282.
Hoekstra PT, Madinga J, Lutumba P, van Grootveld R, Brienen EA, Corstjens PL, van Dam GJ, Polman K, van Lieshout L. Diagnosis of schistosomiasis without a microscope: evaluating circulating antigen (CCA, CAA) and DNA detection methods on banked samples of a community-based survey from DR Congo. Tropical medicine and infectious disease. 2022 Oct 19;7(10):315.
Nikolay B, Brooker SJ, Pullan RL. Sensitivity of diagnostic tests for human soil-transmitted helminth infections: a meta-analysis in the absence of a true gold standard. International journal for parasitology. 2014 Oct 1;44(11):765-74.
Submit a Manuscript:
Copyright © Author(s) 2025. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

