Abstract 001 ASPICON 2025 |September 04 -07 | 2025 |
To Analyze the Performance of Galactomannan Antigen Detection Assay in Cases of Clinically Suspected Pulmonary Aspergillosis
Padmaja Nama1*, Nidhima Aggarwal1, K.Snigdhasri2, Sumit Rai1
1- Department of Clinical Microbiology, AIIMS Mangalagiri, Andhra Pradesh, India.
2- Department of Pulmonary Medicine, AIIMS Mangalagiri, Andhra Pradesh, India.
* Presenting author: padhu9294@gmail.com
Background
Pulmonary aspergillosis is a lung infection caused by the fungus Aspergillus, which is commonly found in the environment. It can lead to different types of disease depending on the person’s health and immune status. Diagnosing Pulmonary aspergillosis early is challenging because of nonspecific radiological and clinical features and occur late in the course of the disease. To improve early diagnosis, non-invasive tests like the Galactomannan antigen detection assay have become important.
Aims & Objectives: To evaluate the diagnostic performance of Galactomannan antigen detection as a screening tool and to isolate Aspergillus species from BAL specimens obtained from patients of clinically suspected Pulmonary aspergillosis.
Material & Method
Prospective observational study was conducted with BAL specimen collected from the patients with clinical and radiological suspicion of Pulmonary Aspergillosis over a period of 45 days. The samples were subjected to direct microscopy and were inoculated onto SDA plates and were incubated at both 25°C and 37°C . Additionally, BAL samples were subjected to GM Rapid Antigen testing, which provides rapid results that can guide early therapeutic intervention while awaiting culture confirmation.
Result
During this study period, BAL of total of 25 patients of suspected cases, tested for GM antigen detection. This assay has increased sensitivity for early detection of Aspergillosis when compared to conventional workflow.
Conclusion
The GM antigen detection assay in BAL fluid is a highly sensitive and reasonably specific tool for diagnosing pulmonary aspergillosis in clinically suspected cases. It is especially valuable for early detection in high-risk, immunocompromised patients, and can guide timely antifungal therapy initiation.
Abstract 002 ASPICON 2025 |September 04 -07 | 2025 |
Tracing the Epidemiological Evidence of Fatal Necrotizing Skin infection by Saksenaea vasiformis through Molecular analysis
Chithra C Nath1*, Nimmy Paul1 ,VinaykumarHallur2, Sreejith Sreekumaran3 , Radhakrishnan E K3
1. Department of Microbiology, Government Medical College, Kottayam, Kerala, India.
2. Department of Microbiology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India.
3. School of Biosciences, Mahatma Gandhi University, Kottayam, Kerala, India.
* Presenting author: chithracnathknpy@gmail.com
Introduction
Saksenaea vasiformis is an emerging non -sporulating zygomycete, mainly causing subcutaneous and disseminated infections with high mortality. As compared to other Mucorales, it causes infection even in an immuno-competent host also.
Materials & Methods
Case history- A 68-year-old male patient with chronic obstructive pulmonary disease presented with 2 weeks duration of fever and breathlessness and 4 days duration of multiple tender slightly warm subcutaneous tender nodules on arms, thighs and back of trunk with surface showing bluish red color. On second day of admission most of these ulcerated and similar new lesions appeared. The case was misdiagnosed and patient was started on antibiotics. A fine needle aspiration cytology from the skin lesion showed non-septate ribbon-like hyphae branching at obtuse angles. The patient deteriorated and died before starting antifungals. The diagnosis was made posthumously.
Isolate was identified by fungal culture and sequencing of the ITS region of the rDNA. Environmental samples were also processed to identify the source of infection.
Results
Saksenaea vasiformis was identified by ITS sequencing. Virulence factors of the isolate was studied by various biochemical tests. Environmental samples also yielded the same pathogen. Phylogenetic analysis of the strains concluded the source of infection.
Discussion and Conclusion
Saksenaea spp. is sometimes missed or causes delay in diagnosis due to its non-sporulating nature. Saksenaea vasiformis,Saksenaea erythrospora are present in environment and cause infections due to insect bite, trauma, contamination of abraded skin etc. Early diagnosis and administration of antifungals can avert the eventual lethal outcome of the disease. ITS sequencing and Phylogenetic analysis help to study the emergence of new species as well as tracing the source of infection.
Chithra C Nath- Department of Microbiology, Government Medical College, Kottayam, Nimmy Paul-Department of Microbiology, Government Medical College, Kottayam, Vinaykumar Hallur- Department of Microbiology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, Sreejith Sreekumaran- Research Scientist B School of Biosciences , Mahatma Gandhi University, Kottayam, Radhakrishnan E K-Associate Professor, School of Biosciences , Mahatma Gandhi University, Kottayam.
Abstract 003 ASPICON 2025 |September 04 -07 | 2025 |
Novel Strategies to Combat Antimicrobial Resistance in the Post-Antibiotic Era: A Narrative Review
Shilpa P*, Sushil Sharma, Madhavrao C, Arup Kumar Misra, Gaurav M Rangari, Srinivasa Rao K
Department of Pharmacology, AIIMS Mangalagiri, Guntur district, Andhra Pradesh, India.
* Presenting author: shilpaprakashpai@gmail.com
Background
The antimicrobial resistance (AMR) has become a “silent pandemic” with many diseases being resistant to the traditional antimicrobials currently present. The limitations of conventional antibiotics and the slow progress in the development of the newer ones necessitate the need for newer innovative multi-targeted strategies.
Aim & Objectives: To review and synthesize key scientific advances in non-conventional strategies to combat the antimicrobial resistance, focusing on newer emerging modalities with novel mechanism of action.
Materials & Methodology
This review evaluates a spectrum of non-conventional antimicrobial modalities and enabling technologies that includes the resurgence of bacteriophage therapy, the development of CRISPR-based antimicrobials, the evolution of antimicrobial peptides (AMPs) and the application of anti-virulence and anti-biofilm agents to disarm pathogens. The diverse strategies examined here represent a vital and expanding pipeline of non-conventional antimicrobials, signifying a major expansion of the therapeutic landscape beyond conventional antibiotics.
Results
• Bacteriophage therapy: Mainly targets the resistant pathogens
• CRISPR – Based antimicrobials : Microbiome sparing action targeting only the disease-causing pathogens enabling targeted eradication
• Antimicrobial peptides: Re-engineered for greater stability, multifunctionality, and reduced resistance induction
• Anti-virulence and anti-biofilm agents: Inhibit bacterial communication (quorum sensing), toxin production, and nutrient acquisition rendering the pathogen harmless and host response eliminating the pathogen naturally.
• Host-directed therapies: Targeting host immune pathways to improve pathogen clearance and reduce immunopathology
• Nanotechnology: Facilitating both intrinsic antimicrobial action and targeted delivery systems
• AI and synthetic biology platforms: Revolutionizing drug discovery through rapid design build test learn cycles
Conclusion
The future of AMR mitigation lies in an integrated, precision-based, and personalized therapeutic framework. These novel strategies promise to reshape infectious disease treatment but require adaptive regulatory, economic, and clinical infrastructure for successful translation into widespread clinical use.
Keywards
Antimicrobial resistance; Bacteriophage therapy; CRISPR-Cas antimicrobials; Antimicrobial peptides; Anti-virulence therapy; Host-directed therapy; Nanotechnology; Artificial intelligence.
Abstract 004 ASPICON 2025 |September 04 -07 | 2025 |
Cryptococcal Lymphadenitis Masquerading as Tuberculosis in an HIV-Positive Patient
Darshan B1,Prasan Kumar Panda2
Department of Internal Medicine (ID Division), All India Institute of Medical Sciences (AIIMS), Rishikesh, India.
* Presenting author: darshanb302@gmail.com
Background
Cryptococcosis is an opportunistic fungal infection predominantly affecting immunocompromised individuals, especially those with advanced HIV/AIDS. While pulmonary and central nervous system involvement are common, lymphadenopathy as the predominant presentation is rare and may closely mimic tuberculosis, resulting in diagnostic delays and inappropriate treatment.
Objectives: To present a rare case of cryptococcal lymphadenitis in an HIV-positive patient initially suspected to have tubercular lymphadenitis, and to highlight the importance of microbiological confirmation prior to initiating antitubercular therapy (ATT) to prevent antimicrobial resistance.
Material & Methodology
A 24-year-old HIV-positive female (CD4 count: 13/μL) presented with high-grade fever, productive cough, significant weight loss, and bilateral cervical and submandibular lymphadenopathy. Chest imaging revealed bilateral centrilobular nodules with tree-in-bud appearance, patchy consolidation, and necrotic mediastinal lymphadenopathy. FNAC from cervical lymph nodes demonstrated numerous encapsulated yeast-like organisms with narrow-based budding, suggestive of Cryptococcus spp., confirmed by periodic acid–Schiff (PAS) and India ink staining. CSF and BAL samples also revealed cryptococcal organisms, with CSF culture confirming Cryptococcus neoformans.
Results
The initial provisional diagnosis of tubercular lymphadenitis was revised to disseminated cryptococcosis. ATT was withheld, and the patient received induction antifungal therapy with liposomal Amphotericin B and Flucytosine. She demonstrated marked clinical improvement and was discharged after completing the induction phase.
Conclusion
This pilot study provides a comprehensive understanding of barriers and facilitators influencing OPAT practices in a resource-poor setting. By addressing these barriers and leveraging facilitators, each healthcare facility can optimize OPAT delivery, improve patient outcomes, and ensure a more efficient and patient-centered approach to antimicrobial therapy. OPAT reduces hospital stays and hospital-acquired infections, is crucial in combating antimicrobial resistance (AMR), and thus directly contributes to integrated antimicrobial stewardship, aligning with a global action plan for AMR in infection prevention and antimicrobial optimal utilization.
Abstract 005 ASPICON 2025 |September 04 -07 | 2025 |
Invasive Fungal Infection Mimicking Sarcoidosis: A Diagnostic Dilemma
Pradeep*, Prasan Kumar Panda, Rajshekhar Lohar
Department of Internal Medicine (ID Division), All India Institute of Medical Sciences (AIIMS), Rishikesh, India.
* Presenting author: pradeep.med24@gmail.com
Background
Sarcoidosis is a granulomatous disease with multisystem involvement with variable clinical presentation. It can mimic infectious diseases, malignancy and other autoimmune diseases. Among these invasive fungal infections, those caused by Aspergillus species pose significant diagnostic challenges in resource-limited settings.
Uniqueness of the case: This case report describes an unusual case of invasive fungal infection mimicking sarcoidosis and lymphoma.
Case Presentation
A 41-year-old immunocompetent male presented with intermittent fever for 2.5 months, weight loss, abdominal pain and dry cough. Imaging showed hepatosplenomegaly with multiple hypo-enhancing lesions and mediastinal and abdominal lymphadenopathy. Elevated serum ACE levels (73 U/L) and non-necrotic lymphadenopathy on PET-CT pointed toward sarcoidosis. EBUS-TBNA was inconclusive, showing only reactive lymphadenitis. Steroids were initiated empirically. Subsequent fungal culture from the EBUS-TBNA specimen grew Aspergillus fumigatus, confirming invasive fungal infection. Steroids were stopped, and antifungal treatment commenced.
Discussion and Conclusion:
Invasive fungal infections can mimic sarcoidosis both radiologically and biochemically. This case highlights the importance of establishing a tissue diagnosis before starting immunosuppressive therapy. A thorough evaluation, including fungal cultures, is essential to avoid diagnostic pitfalls and therapeutic adverse effects.
Abstract 006 ASPICON 2025 |September 04 -07 | 2025 |
A Retrospect Record Based Study of Bacteriological Isolates from Stool Samples : A Tertiary Care Hospital Study in Goa
Vijayalakshmi Gujapaneni*, Anita Sandhya Estibeiro
Department of Microbiology, Goa Medical College, Bambolim, Goa, India.
* Presenting author: drvijayadeepak@gmail.com
Background
Diarrhoea is one of the major public health concern at the international level, mainly in developing countries like India. They remain the major contributors to acute enteric infections and diarrhoea mainly in children and in adults.
Aims & Objectives: This study aims to isolate the pathogens from stool specimens of diarrhoeal cases and to determine the antimicrobial susceptibility pattern in tertiary care setup which includes inpatients and outpatients.
Materials & Methodology
An Institutional based Retrospective Cross-sectional study was carried out among 837 members which includes both children and adult population with diarrhoea from January 2025 to June 2025 in Goa.
Method of Analysis: Stool specimen was collected from all participants who presented with diarrhoea. A wet mount preparation was done and looked for the presence of RBCs, Pus cells and any other parasites/ eggs/ larvae.
Identification of Growth: Specimen was processed for the identification of Salmonella, Shigella and Vibrio species using MacConkey agar, Xylose Lysine Deoxycholate agar, Thiosulphate Citrate Bile salts Sucrose agar and further Biochemical tests done. The antimicrobial susceptibility pattern of isolates was performed using the Kirby-Bauer disc diffusion technique. The data was entered into Biomerieux VITEK 2 release version 9 for confirmational identification of species.
Results
A total of 837 samples were collected, in which 248 were males (29.6%), 318 were females (37.9%) and 271 were children (32.3%) over a period of 6 months from January to June. 15 samples showed Salmonella and Shigella. Vibrio species were not isolated. Salmonella cases were 7(46.6%) and Shigella were 8 cases (53.3%). Majority of the infected patients belong to pediatric age group.
Antibiotic sensitivity: Among Salmonella isolates, highest Sensitivity was observed to Levofloxacin (86%), Ciprofloxacin (88%), and Azithromycin (75%). Resistance was seen to Ampicillin (82%), Chloramphenicol (78.9%) and Cotrimoxazole (57.2%).
Most of the Shigella isolates were sensitive to Ciprofloxacin (88%),Levofloxacin(82%) and Meropenem (72%), and resitant to Ampicillin (75%), Tetracycline (72%), Cotrimoxazole (69%) and Chloramphenicol (62%). Multi-drug resistance was noted in 2 (98.57%) and 1 (92.5%) of Salmonella and Shigella cases.
Conclusion
Out of 837 samples analysed, 7 samples were positive for Salmonella of which 3 were from pediatric age group, 1 from geriatric age group and 3 from middle age group. 8 samples were positive for Shigella of which 5 samples were from Pediatric age group and 3 samples from middle age group. Was equally distributed among both genders.
Keywords: Diarrhoea; Salmonella; Shigella; Antimicrobial Susceptibility.
Abstract 007 ASPICON 2025 |September 04 -07 | 2025 |
From Swab to Spectrum: A Study of Ear Pathogens and Their Antimicrobial Resistance Pattern in a Tertiary Care Centre
Navi Nallasamy* , Ravish Kumar M, Saraswathi MP, Jyotismita Rabongshi, Lavanya P.
Department of Microbiology, ESIC Medical College and Hospital, K.K Nagar, Chennai, Tamil Nadu, India.
* Presenting author: drnavi324@gmail.com
Background
Otitis and other ear infections are common clinical presentations in ENT practice. With the increasing burden of multidrug-resistant organisms, accurate identification of causative pathogens and their resistance profiles is crucial for guiding empirical therapy. Continuous monitoring is therefore essential in tertiary care hospitals.
Aims & Objectives: To determine the spectrum of pathogens causing ear infections and to study their antimicrobial resistance patterns, with a focus on Pseudomonas species, the most common isolate.
Material & Methodology
Study: A prospective observational study was conducted over six months (Jan–Jun 2025) in the Department of Microbiology, ESIC Medical College and Hospital, K.K Nagar, Chennai.
Sample size: 61 patients presented with signs of ear infections.
Sample collection: Ear swabs were collected under aseptic precautions.
Processing: Standard microbiological techniques like specimen collection, direct microscopy, primary culture, biochemical/automated identification methods and AST were done.
Identification: Isolates identified up to species level.
Antimicrobial Susceptibility Testing (AST): Performed using the Kirby–Bauer disk diffusion method, interpreted as per recent CLSI guidelines.
Result
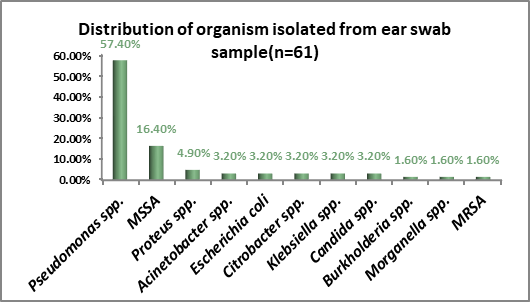
Out of 61 ear swab samples, the following organisms were isolated:
Resistance pattern in Pseudomonas isolates (n=35):
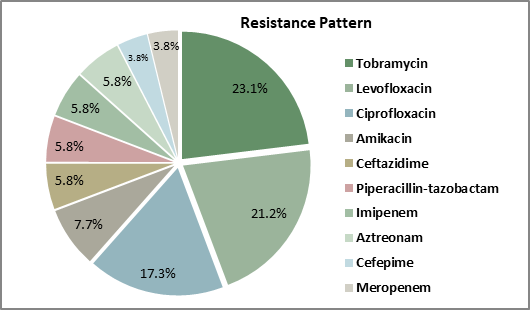
Conclusion
Pseudomonas species was the predominant pathogen in ear infections in this cohort, exhibiting considerable resistance to aminoglycosides and fluoroquinolones. The identification of multidrug-resistant isolates, including MRSA and non-fermenting Gram-negative bacilli, underscores the need for continuous surveillance, judicious antibiotic use, and effective antimicrobial stewardship programs to improve patient outcomes. Encouraging rational prescribing practices and enhancing awareness are vital to slow the progression of resistance. Therefore, regular audits are indispensable to uphold quality standards within the healthcare system.
Abstract 008 ASPICON 2025 |September 04 -07 | 2025 |
Rationality Assessment Tool-Based Assessment of Antimicrobial Prescriptions: Findings from a Multicentric Point Prevalence Survey in India
Naveen Murali1*, Soumya vij1, Ashish Kakkar1, Nusrat Shafiq1, Rachna Rohilla2, Shilpa N.Kaore3, Deepak Kumar4, Shefali Gupta5, Nisha Sharma1, Aayudhin Menon1, Tania Sidana1, Rupamdeep kaur1
1- PGIMER, Chandigarh, India.
2- AIIMS, Bathinda, Punjab, India.
3- AIIMS Bhopal, Madhya Pradesh, India.
4- AIIMS Jodhpur, Rajasthan, India.
5- AIIMS, Raebareli, Uttar Pradesh, India.
* Presenting author: drnaveenpgi@gmail.com
Background
Point Prevalence Surveys (PPS) play a vital role in assessing antibiotic use and prescribing practices. This substudy uses the Antimicrobial Rationality Assessment Tool (AmRAT-2.0) to assess prescription rationality across five participating tertiary care hospitals in India.
Aims & Objectives: To evaluate the rationality of systemic antimicrobial prescriptions in tertiary care hospitals across India. To identify inappropriate prescribing patterns with respect to antibiotic choice, dose and duration
Material & Methodology
This substudy was carried out as part of the PPS, including medical, surgical and intensive care units. Patterns of antimicrobial use with indications, purpose, rationality assessment (according to the AmRAT 2.0 tool) and isolated pathogens were evaluated by the site team. At the second level, two experts (with nearly 5 years of experience in audit and feedback) reviewed the observations using the same tool in a blinded manner.
Results
Across the five sites, a total of 495 prescriptions were evaluated, of which 379 (77%) were found to be rational and 116 (23 %) were assessed as irrational at the level of the participating site. Among the irrational prescriptions, 72 (62%) had an incorrect choice, 35 (30%) had an incorrect dose, and 53 (45%) had an incorrect duration of therapy. There was concordance between the site-level and Level 2 assessments in 373 (75%) prescriptions.
Conclusion
Significant inter-site variability in prescription appropriateness was observed, highlighting the need for: Audit-feedback, Strengthening of institutional antibiotic guidelines, and Incorporating AmRAT-based periodic audits can help improve antimicrobial use practices.
Abstract 09 ASPICON 2025 |September 04 -07 | 2025 |
Impact of Multidrug-Resistant Organisms on Routine Antibiograms of Blood Culture and the Role of Improper Blood Culture Collection
Kanika Charan*, Fatima Khan, S. Zeeshan Hashmi, Mohammad Anas Mazhar Aziz, Harsha Suresh Mathew, Asfia Sultan, Anees Akhtar
Department of Microbiology, JNMCH, AMU, Aligarh, Uttar Pradesh, India.
* Presenting author: kanikacharancomjnmh@gmail.com
Background
Blood culture is a critical diagnostic tool for identifying bloodstream infections and guiding antimicrobial therapy. However, improper blood collection techniques can significantly compromise the quality of results, leading to contamination, false-positive growth, or underrepresentation of true pathogens. This not only skews routine antibiogram data but may also contribute to the apparent rise in multi-drug resistant organisms (MDROs).
Objectives : To evaluate the impact of MDROs on routine antibiogram and the reliability of routine antibiogram and to assess the role of improper sampling .
Material & Methodology
A retrospective analysis of blood culture reports and antibiograms over six months was performed to identify the frequency of MDROs and their correlation with documented contamination rates . When MDRO is reported as a hospital contaminant, it indicates that the multidrug-resistant organism was likely introduced during sample collection or handling often due to poor infection control or environmental contamination rather than being the true cause of infection, and may not reflect the patient’s clinical condition. Concurrently, A structured questionnaire-based survey was conducted among healthcare professionals involved in sample collection across various departments. Questions focused on knowledge and adherence to standard blood culture collection protocols, including skin antisepsis, volume of blood, timing, and number of sets collected .Thumbprints of 30 residents and healthcare workers were collected before and after handwashing from different wards to assess hand hygiene effectiveness.
Results
A total of 335 blood culture isolates were analyzed , of which 43 isolates (12.83%) were identified as multidrug-resistant organisms (MDROs), while the remaining 292 isolates (87.16%) were classified as non-MDROs . Among the predominant organisms, Escherichia coli and Klebsiella species exhibited notable variations in antimicrobial susceptibility patterns between MDRO and non-MDRO groups.
For Escherichia coli, Meropenem susceptibility was observed to be 80% among non-MDRO isolates, compared to 41.4% overall, including MDROs. Gentamicin susceptibility was observed at 66.7% in non-MDROs, decreasing to 34.5% overall, including MDROs . Similarly, Ceftriaxone susceptibility was observed at 53.3% in non-MDROs and 17.2% in MDROs. Levofloxacin susceptibility remained consistently low across both groups, observed at 6.6% in non-MDROs and 3.4% in MDROs.
For , Klebsiella species Meropenem susceptibility was observed at 55% in non-MDRO isolates and 21% overall, including MDROs. Piperacillin-Tazobactam susceptibility was reported at 36.3% in non-MDROs and 14% overall, including MDROs. Susceptibility to Ceftriaxone and Levofloxacin remained low in both groups, observed at 9.1% in non-MDROs and 3.6% overall, including MDROs.
The survey revealed variable adherence to standard blood culture collection protocols, with notable gaps in hand hygiene, use of antiseptics, and training. Only 50% of respondents identified the correct blood culture collection site, while 75% used the recommended antiseptic and sterile gloves. Despite 80.6% practicing hand hygiene, just 27.8% had received formal training highlighting critical gaps that may impact culture quality and antibiogram reliability .
Thumbprint cultures from 30 residents showed microbial growth even after handwashing
Conclusion
Routine antibiograms are at risk of distortion, leading to inappropriate empirical antibiotic use. Inadequate blood culture collection affects result accuracy and may inflate MDRO prevalence. Strengthening training, protocol adherence, and hygiene enforcement to improve diagnostic reliability and antimicrobial stewardship.
Keywords: Blood culture; Multidrug-resistant organisms (MDROs); Antibiogram; Sample contamination; Hand hygiene; Antimicrobial resistance.
Abstract 010 ASPICON 2025 |September 04 -07 | 2025 |
Antimicrobial Susceptibility of Fosfomycin in Uropathogens from Nephrology and Urology Patients at a Tertiary Care Center
K. Yamini*, S. Likhitha, R. Jayaprada, JP. Joshi Sowmya
Department of Microbiology, SVIMS –SPMC(W), Tirupati, India.
* Presenting author: yaminikurapati@gmail.com
Background
Urinary tract infections (UTIs) are among the most frequently encountered community-acquired infections by healthcare professionals. Currently, nitrofurantoin is often prescribed empirically for lower UTIs. However, widespread and improper use of antimicrobial agents has led to a rise in multidrug-resistant (MDR) uropathogens. According to existing literature, fosfomycin emerges as a potential alternative treatment option against MDR pathogens.
Aims & Objectives: To assess the susceptibility pattern of Fosfomycin among Multidrug-Resistant (MDR) and Extended Spectrum β-Lactamase (ESBL) producing uropathogens isolated from patients in the Nephrology and Urology departments.
Material & Methodology
We conducted a retrospective review of culture reports for uropathogens isolated from the Nephrology and Urology departments between July 2023 and June 2025. Urine samples were inoculated onto MacConkey agar and nutrient agar plates using a calibrated loop and incubated aerobically at 37°C for 24 hours. A single colony count exceeding 10^5 CFU/mL of urine was deemed significant. Following identification through biochemical tests, antibiotic susceptibility testing was performed using the Kirby–Bauer disc diffusion method. Bacterial suspensions standardized to 0.5 McFarland were inoculated onto Mueller-Hinton agar plates, and testing was carried out in accordance with Clinical and Laboratory Standards Institute (CLSI) guidelines.
Results
Significant growth of pathogenic bacteria was observed in 2814 samples out of 10,524 urine samples from nephrology and urology departments. A breakdown of 2814 culture positives showed 40.15% susceptibility towards Fosfomycin. Among these 1817(65%) are Multidrug resistant (MDR) organisms, 358(12.7%) are Extended Spectrum β Lactamase (ESBLs) producers, 407(14.4%) are Carbapenem resistant Enterobacteriaceae (CREs) were isolated. Fosfomycin showed 37.3% susceptibility towards MDROs, 43.2 % towards ESBLs, 40.05% towards CREs.
Conclusion
Our results demonstrated that Fosfomycin exhibited a higher susceptibility rate compared to other antimicrobials against the uropathogens identified in our study. The use of high-level antibiotics contributes to an increased burden of antimicrobial resistance through selective pressure. Given the limited availability of alternative treatment options for these resistant pathogens, Fosfomycin—available in oral form, administered as a single dose, and showing minimal cross-resistance to other antibiotics—may serve as a viable alternative therapy for uncomplicated lower urinary tract infections.
Keywords: Antimicrobial resistance, Fosfomycin, Urinary tract infections
Abstract 011 ASPICON 2025 |September 04 -07 | 2025 |
PLHIV: A Complex Interplay of Polymicrobial Infections Including Syphilis, Tuberculosis, Cryptococcosis, and Herpes Simplex
Anika Malviya*, Prasan Kumar Panda
Department of Internal Medicine (ID Division), All India Institute of Medical Sciences (AIIMS), Rishikesh, India.
* Presenting author: anikamalviya0805@gmail.com
Introduction
People living with HIV (PLHIV) are predisposed to multiple opportunistic infections owing to severe immunosuppression. Central nervous system (CNS) infections such as tuberculosis, cryptococcosis, neurosyphilis, and herpes simplex virus (HSV) disease often present with overlapping features, making timely and accurate diagnosis difficult. Polymicrobial involvement adds further complexity, especially in settings with limited access to advanced microbiological or molecular diagnostics.
Case Discussion
We describe a 28-year-old man with advanced HIV infection (CD4 count: 51/µL) who presented with fever, genital ulcers, altered sensorium, and right hemiplegia. The presence of genital ulcers and reactive RPR with supportive CSF findings suggested neurosyphilis, and ceftriaxone therapy was initiated. Brain imaging revealed multiple ring-enhancing lesions, interpreted initially as tuberculomas, prompting anti-tubercular therapy. However,patient had persistent fever, persistently positive serum cryptococcal antigen along with new-onset seizures necessitated reconsideration, leading to the diagnosis of disseminated cryptococcosis with CNS cryptococcomas. Antifungal therapy with liposomal amphotericin B, flucytosine, and subsequently fluconazole was administered. Concurrent herpes labialis and genital herpes were treated with acyclovir.He developed Trimethoprim – Sulfamethoxazole induced pancytopenia for which it was discontinued.During the course, the patient developed aspiration pneumonia requiring intensive supportive care. A coordinated, multidisciplinary management strategy eventually achieved clinical stabilization.
Conclusion
This case illustrates the diagnostic and therapeutic challenges of polymicrobial CNS infections in PLHIV. The overlapping clinical and radiological manifestations of cryptococcomas and tuberculomas highlight the need for repeated diagnostic reassessment. Tailored antimicrobial therapy and multidisciplinary input are key to favorable outcomes. Vigilance for concurrent infections must remain a cornerstone in the management of advanced HIV, as timely recognition significantly impacts prognosis.
Abstract 012 ASPICON 2025 |September 04 -07 | 2025 |
Breast Lump Caused by Dirofilaria Repens: A Rare Cause of the ‘Dancing Sign’ and an Overlooked Differential in Subcutaneous Nodules
Nikhil John1*, Muruganand M2, Boppe Appalaraju2, N Elango2
1- All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India..
2- PSG Institute of Medical Sciences and Research, Coimbatore, Tamilnadu, India.
* Presenting author: drnikhiljohn.cmid@gmail.com
Background
Human dirofilariasis is a mosquito-borne zoonotic infection caused primarily by Dirofilaria repens in the Indian subcontinent. The primary definitive hosts for Dirofilaria repens are domestic and wild canids, including dogs, foxes, and wolves, which harbor the adult worms and produce microfilariae. Humans are accidental hosts and are infected by mosquitoes carrying the larvae. The infection most commonly presents as isolated subcutaneous or ocular nodules. Systemic involvement is rare. Breast involvement is uncommon and can mimic neoplastic lesions, leading to diagnostic dilemmas. A well-known ultrasonographic feature in parasitic breast nodules is the “dancing sign,” traditionally associated with Wuchereria bancrofti. This sign, however, is not pathognomonic and can mislead diagnosis if other filarial species are not considered.
Novelty/Uniqueness of the Case
This case describes a rare instance of Dirofilaria repens infection presenting as a breast lump with internal motility on ultrasonography. The detection of both adult worms and peripheral microfilariae, with confirmatory species-specific PCR, makes this a diagnostically significant case. The demonstration of classic morphological features of D. repens in both adult and microfilarial forms highlights the importance of microscopy in endemic settings. The case emphasizes that D. repens should be considered in the differential diagnosis of parasitic breast lesions, especially in areas where zoonotic filariasis is prevalent.
Case History
A 53-year-old postmenopausal woman (P2L2), with a history of hypertension and type 2 diabetes mellitus, presented with a painless, slowly growing lump in the upper outer quadrant of her right breast, measuring approximately 2 × 2 cm. She denied any history of trauma, fever, or systemic symptoms. There was no personal or family history of malignancy. She apparently noticed the lesion one month back. Ultrasonography revealed a hypoechoic lesion with internal undulating movements—referred to as the “dancing sign.”
Surgical excision of the lump under local anesthesia was performed. On immersion of the tissue in distilled water, multiple actively motile adult worms were observed emerging spontaneously, suggesting a parasitic etiology.
Microscopy Findings
Adult Worm Morphology (Direct Light Microscopy):
Long, slender, cylindrical worms with tapered ends.
Cuticle demonstrated prominent longitudinal ridges and fine transverse striations, creating a serrated external appearance—a characteristic feature of Dirofilaria repens.
Internal structures included a digestive tract and reproductive organs.
No sheath or external ornamentation seen, ruling out other sheathed filarial worms.
Peripheral Blood Smear (Post-DEC Provocation, Giemsa stain):
Unsheathed microfilariae, measuring ~300–370 µm in length.
Smooth, curved body with a tapered anterior end and a blunt tail.
Somatic nuclei did not extend to the tail tip, a classic feature of D. repens microfilariae.
Background was clean, with minimal inflammatory and eosinophilic reaction.
Discussion & Conclusion
This case reinforces the critical insight that the “dancing sign” on breast ultrasonography, though classically attributed to Wuchereria bancrofti, may also be produced by Dirofilaria repens. Accurate morphological identification of the worm and its microfilariae is crucial. The presence of adult worms in the excised tissue and provoked peripheral microfilaremia confirmed the diagnosis. PCR testing further established species identity:
Forward primer: 5′-CGGGATCCAACATGGCTATTATTC-3′
Reverse primer: 5′-CGGAATTCCTAGCCGTTTGAAACAC-3′
PCR from the adult worm confirmed D. repens, while PCR and antigen detection for W. bancrofti were negative, supporting a diagnosis of localized zoonotic dirofilariasis.
The patient was treated postoperatively with Diethylcarbamazine (DEC) at 6 mg/kg/day in three divided doses for 21 days to eliminate residual microfilariae. She remained asymptomatic at subsequent follow-up.
This case highlights the importance of maintaining a high index of suspicion for zoonotic filarial infections in unusual anatomical sites. In endemic regions, parasitic infections should be considered early in the differential diagnosis of mobile subcutaneous or breast nodules to prevent misdiagnosis and unnecessary interventions.
Keywords: Dirofilaria repens; Breast lump; Dancing sign; Zoonotic filariasis.
Abstract 013 ASPICON 2025 |September 04 -07 | 2025 |
Importance of Diagnostic and Antimicrobial Stewardship in the Management of Invasive Pulmonary Mucormycosis: A Case Report
Anusha B*, Munesh Kumar Gupta, Ragini Tilak, Kanupriya Tiwari, Deepak Kumar Shah
Institute of Medical Sciences,Banaras Hindu University,Varanasi, India.
* Presenting author: anushabalakrishnan2509@gmail.com
Background
Invasive pulmonary mucormycosis is a life-threatening fungal infection, where prompt diagnosis with immediate report communication is a need. Moreover, such cases are to be managed by a multidisciplinary team. We present a case of probable invasive pulmonary mucormycosis case in a diabetic male
Aims & Objectives: To highlights the following:
1. Appropriate sample collection
2. Reduce TAT for direct microscopy
3. Need for prompt reporting of direct microscopy results.
4. Administration of amphotericin B and withdrawal of voriconazole
Case history
A 50-year-old male presented to Department of Tuberculosis and Respiratory Medicine with the complaint of cough with sputum production for one month, hemoptysis for 20 days, breathlessness for 15 days, and left-sided chest pain for 7 days. Routine investigations revealed Hb1Ac of 11, TLC 11000, 88% neutrophil. HRCT thorax revealed thick peripheral rim of consolidation with ground glass opacities(reverse halo sign), adjacent interlobular septal thickening in left lower lobe of left lung with mild pleural effusion with fissural extension. There were no AFB and fungal elements in the sputum sample. However, broad-aseptate hyphae were observed in the KOH wet mount of BAL sample. The report were communicated to the concerned consultant and they withdrew voriconazole and administed amphotericin B. Raised blood sugar was managed by administration of sc inj Insulin. Moreover, on endoscopy, PNS revealed a black-scar over the middle turbinate of the left nostril. The patient pulmonologist, CTVS & ENT surgeon, endocrinologist is admitted and being managed by a multidisciplinary team comprising, radiologist and microbiologist.
Discussion and Conclusion
Strong suspicion of pulmonary mucormycosis in diabetic patients presenting with hemoptysis should be there. Here, appropriate sample should be sent for microbiological evaluation. Moreover, prompt diagnosis and communication with management by a multidisciplinary team should be done to reduce the morbidity and mortality
Abstract 014 ASPICON 2025 |September 04 -07 | 2025 |
Bacteriological Culture Profile of Isolates from Urine Samples: A 6 Month Retrospective Study in A Tertiary Care Hospital in Goa
Navita Naik*, Anita Sandhya Estibeiro
Department of Microbiology, Goa Medical College, Bambolim- Goa, India.
* Presenting author: naiknavita9@gmail.com
Background
Urinary tract infection is common microbial infection in all ages and sexes. It is the most common bacterial infection acquired in the community and hospitals. Although generally self- limiting, treatment with antibiotic leads to rapid resolution of symptoms.
Objective: The present study was undertaken to determine the urinary tract infection caused by bacterial isolates in a tertiary care hospital including admitted patients of all age groups and gender. Urine samples were tested in the microbiology department and antimicrobial susceptibility was noted.
Material & Methodology
The study was done over a period of 6 months from January to June 2025 using Biomerieux VITEK 2 release version 9. The isolates were tested and the antimicrobial susceptibility was noted.
Result
A total number of 10,957 samples of urine were tested over the study period out of which 1826 showed growth of isolates (16%)
The organisms which were isolated were Escherichia coli (35.44%), Klebsiella species (28.05%), Citrobacter species (5.69%), Acinetobacter species (5.20%), Pseudomonas aeruginosa (9.58%), Enterococcus species (14.62%) and Proteus mirabilis (1.36%).
The antibiotic susceptibility for Gram positive organisms shown was Vancomycin (67.41%), Linezolid (65.16%), Ciprofloxacin (57.68%), Tetracycline (41.57%), Nitrofurantoin (25.46%). The antibiotic susceptibility for Gram negative bacteria shown was Meropenem (46%), Nitrofurantoin(37.22%), Chloremphenicol (34.17%), Co-triamoxazole (28.05%),Ceftriaxone(18%).
The study included 27.49% patients from Surgery department wards, 35.15% from Medicine department wards, 25.73% from Obstetrics and Gynaecology wards of which antenatal were 17.46% and 10.5% from Paediatric wards.
64.44% of female patients were infected and 35.56% of male patients.
Conclusion
Urinary tract pathogens can infect all age groups. Females were infected more than males .Antenatal population also showed high infectivity rates and hence needs timely treatment with appropriate antibiotics to avoid complications.
Keywords: Antibiotic susceptibility; Escherichia coli; klebsiella; Acinetobacter; Citrobacter; Enterococcus; Proteus Mirabilis.
Abstract 015 ASPICON 2025 |September 04 -07 | 2025 |
Clinical Pharmacologists as the Cornerstone of Antimicrobial Stewardship in India: A Policy to Practice Perspective
Sree Sudha T Y1*, Pugazhenthan Thangaraju2, Sumit Kumar Mahato1
1- Department of Pharmacology, All India Institute of Medical Sciences, Deoghar, Jharkhand, India.
2- Department of Pharmacology, Jharkhand, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
* Presenting author: sudhambbs2010@gmail.com
Background
Antimicrobial resistance (AMR) has been called one of the most critical threats to public health in the modern era, significantly influencing morbidity, mortality, and economic costs globally. In India, the challenge is acute due to an extensive infectious disease burden combined with high rates of antimicrobial misuse and a healthcare system where insurance coverage is below 15%, leaving most patients to pay out of pocket. AMR rates are especially alarming for pathogens like Escherichia coli and Klebsiella pneumoniae, with up to 84% fluoroquinolone resistance and nearly 59% carbapenem resistance reported. Clinical pharmacologists, with expertise in drug dynamics and pharmacotherapeutics, have become central to these stewardship missions, especially in countries navigating significant systemic and infrastructural challenges, such as India.
Case Discussion
Policy Framework and Implementation: India’s national battle with AMR is anchored by policies like the National Action Plan on AMR (NAP-AMR), which fosters multi-sectoral engagement and stricter antibiotic controls. Kerala’s Public-Private Partnership (PPP) stands out as a successful regional AMS model, coordinating public/private healthcare and customizing guidelines to match local resistance trends. Despite sophisticated policymaking efforts, implementation barriers—such as inconsistent leadership responsibility, gaps in laboratory infrastructure, and limited regulatory enforcement—persist at the institutional level .
Role and Impact of Clinical Pharmacologists:
Clinical pharmacologists have emerged as essential team members bridging these gaps. Their skillset allows them to tailor antimicrobial regimens based on pharmacokinetic and pharmacodynamic principles, especially for vulnerable populations like ICU patients and neonates. Additionally, they are integral to collaborative, multidisciplinary stewardship teams, often acting as coordinators among infectious disease physicians, microbiologists, and pharmacists, and serving as educators for rational antibiotic use. They influence hospital policy by managing formularies, developing antibiotic restriction policies, and leading audit-feedback cycles to optimize prescribing practices. Evidence shows that their involvement drives more appropriate antibiotic use and improved patient outcomes.
Barriers and Best Practices:
Key challenges include a shortage of trained clinical pharmacologists and limited formal AMS education for clinicians, which restrict sustainable program growth. Diagnostic limitations such as insufficient laboratory services – further complicate timely, targeted antimicrobial therapy.
Nonetheless, positive case studies highlight clinical pharmacologists’ value:
The Kerala Public–Private Partnership illustrates how stakeholder engagement, coordinated training, and localized guidelines translate to better stewardship and guideline adoption.
In one tertiary hospital’s NICU program, clinical pharmacologist leadership directly led to decreased antibiotic use and lower mortality and sepsis rates over just six months.
In a South Indian ICU, consultative stewardship involving clinical pharmacologists reduced inappropriate prescriptions by over 70%.
Conclusion
Clinical pharmacologists stand at the interface of AMR policy and practice, bringing specialized expertise necessary for the design, implementation, and assessment of AMS programs in India. While innovative state and institutional models showcase their impact, the road ahead includes overcoming persistent educational, infrastructural, and cultural obstacles. Multi-sector collaboration, robust regulatory mechanisms, and the digital transformation of AMS processes will be vital for future progress. Empowering this cadre is critical for safeguarding the effectiveness of antimicrobials and advancing patient care outcomes nationwide.
Abstract 016 ASPICON 2025 |September 04 -07 | 2025 |
Phage-Antibiotic Combination for Multidrug -Resistant Infections: A Systematic Review of Preclinical and Clinical Evidence
Boda Srikanth Nayak*, Sushil Sharma, Madhavrao C, Gaurav Manikrao Rangari, Arup Kumar Misra, Srinivasa Rao Katiboina
Department of Pharmacology, AIIMS Mangalagiri, Andhra Pradesh, India.
* Presenting author: bodasrikanthnaik@gmail.com
Background
The rising prevalence of multidrug-resistant (MDR) bacteria poses a critical threat to public health. Bacteriophage therapy, which uses viruses that selectively infects and lyses bacteria, re-emerged as a potential adjunct to antibiotics. Phages are specific to bacterial hosts, replicates at infection sites, and degrades biofilms. Preclinical and clinical evidence suggested that combining phages with antibiotics enhances bacterial eradication and reduces resistance development, known as phage–antibiotic synergy. However, the efficacy and safety of this combination remained incompletely characterized.
Aims & Objectives: This systematic review aimed to evaluate whether adjunctive phage therapy improves clinical and microbiological outcomes compared to antibiotic therapy alone in MDR infections, using evidence from animal and human studies.
Material & Methodology
A comprehensive search of PubMed, EMBASE, MEDLINE and SCOPUS was conducted and selected articles published from inception of time to till July 2025,studies on combined phage–antibiotic therapy against MDR bacterial infections are considered for screening. Eligible studies of randomized controlled trials, non-randomized comparative studies, cohort studies, case series, and controlled animal experiments were included. Dual independent reviewers screened the studies & extracted the data on study characteristics, antibiotic regimens, outcomes. Primary outcomes were clinical improvement and microbiological eradication; secondary outcomes included mortality, time to resolution, resistance emergence, and adverse events.
Result
Total results were compiled after the screening of total 2833 articles according to our search strategy. All the studies reported clinical improvement in 78–93% of patients and microbiological eradication in 61–87%, with evidence that phages resensitized bacteria to previously ineffective antibiotics. However, the evidence base largely consisted of small case series and compassionate use reports, with few randomized trials. Considerable heterogeneity existed in phage types, dosing schedules, administration routes, and antibiotic regimens.
Conclusion
This review synthesized the existing evidence on phage–antibiotic combination therapy for MDR infections, highlighting its therapeutic potential and limitations, and identified methodological gaps to guide future well-designed studies.
Abstract 017 ASPICON 2025 |September 04 -07 | 2025 |
In Vitro Activity of Ceftaroline Against Methicillin-Resistant Staphylococcus aureus (MRSA)
Virendra Kumar Jaiswar*, Sanjay Biswas, Gaurav Salunke, Shamita Binod, Anil Kumar Verma, Priyanka Singh, Shradha Kamble,
Department of Microbiology, Tata Memorial Hospital, Mumbai, Maharastra, India.
* Presenting author: vbj13670@gmailcom
Background
Methicillin-resistant Staphylococcus aureus is a major cause of hospital-acquired infections, contributing significantly to morbidity, mortality, prolonged hospital stays, and increased healthcare costs. Ceftaroline, a fifth-generation broad-spectrum cephalosporin, has been approved by the FDA for the treatment of community-acquired pneumonia and ABSSSI caused by susceptible organisms, including MRSA. This study evaluates the in vitro activity of Ceftaroline against MRSA isolates from hospitalized patients.
Aims & Objectives:
1. To evaluate the in vitro activity of Ceftaroline against MRSA isolates obtained from pus, abscess, aspirate, or tissue samples from patients diagnosed with ABSSSI.
2. To compare the susceptibility of MRSA to Ceftaroline with other commonly used antibiotics, including Vancomycin, Linezolid, Teicoplanin, and Daptomycin.
Material & Methodology
1. MRSA screening was performed using the Cefoxitin (30 µg) disc diffusion method as per CLSI guidelines.
2. Identification of S.aureus and antimicrobial susceptibility testing (Vancomycin, Linezolid, Teicoplanin, and Daptomycin) were carried out using the VITEK-2 system.
3. Susceptibility to Ceftaroline was determined using the E-test method, following CLSI standards.
Results
Among the tested isolates, only 49.2% showed a MIC of ≤ 0.5 µg/mL for Vancomycin, and 95% exhibited an MIC of 2 µg/mL for Linezolid. In contrast, the percentage of MRSA isolates with MIC values of ≤ 0.5 µg/mL was significantly higher for the other agents: Teicoplanin (100%), Ceftaroline (92.5%), and Daptomycin (90.98%).
Conclusion
Ceftaroline demonstrated superior in vitro activity against MRSA compared to Vancomycin, with a higher proportion of susceptible isolates. These findings suggest that Ceftaroline could serve as a promising therapeutic alternative for the management of MRSA-related infections, particularly in cases of ABSSSI.
Abstract 018 ASPICON 2025 |September 04 -07 | 2025 |
Lenacapavir in HIV Management: A New Era of Antiretroviral Therapy: A Narrative Review
Subalakshmi R*, Madhavrao C, Sushil Sharma, Srinivasa Rao K, Gaurav Rangari, Arup Kumar Misra
Department of Pharmacology, All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India.
* Presenting author: suba4062@gmail.com
Background
HIV remains a major global public health issue. As of the end of 2024, around 40.8 million people were living with HIV, with 1.3 million newly diagnosed cases. Despite the availability of drugs for HIV therapy, the development of new agents remains essential due to the emergence of drug resistance. Lenacapavir, the first-in-class capsid inhibitor, targets the viral capsid through a novel mechanism distinct from other drug classes. It was recently approved for pre-exposure prophylaxis and is also used in combination with other antiretroviral agents for the treatment of multidrug-resistant HIV-1.
Aims & Objectives: To provide a comprehensive overview of Lenacapavir, focusing on its pharmacological properties, clinical trial evidence, safety and efficacy.
Material & Methodology
A literature search was performed using PubMed, Scopus, and EMBASE to identify publications available up to June 2025. The search terms included “lenacapavir,” “HIV capsid inhibitor,” “antiretroviral therapy,” “multidrug-resistant HIV,” and “pre-exposure prophylaxis.” Both clinical trials and review articles were considered eligible for inclusion. Only articles published in English were reviewed
Results
Lenacapavir acts by targeting the HIV capsid, disrupting multiple stages of the viral lifecycle including proviral integration, viral assembly, and release—ultimately leading to non-infectious viral particles. Its oral formulation has low bioavailability with a half-life of 10–12 days, whereas the subcutaneous depot formulation supports biannual dosing due to its prolonged half-life of 8–12 weeks and a Tmax of approximately 80 days. The drug is >98% protein-bound and primarily eliminated unchanged in feces, undergoing minor CYP3A and UGT1A1 metabolism. Plasma levels are reduced by CYP3A4 inducers. In the Phase 3 CAPELLA trial, lenacapavir achieved a ≥0.5 log₁₀ viral load reduction in 88% of participants by Day 14 and maintained viral suppression in 81–83% through Week 52, even with limited background therapy. Resistance mutations (e.g., M66I, Q67H) were observed primarily in the context of poor adherence. The Phase 2 CALIBRATE study in treatment-naïve individuals showed 85–90% suppression at Week 54. In the PURPOSE trials, lenacapavir administered every six months for PrEP demonstrated up to 96% reduction in HIV incidence, with mild injection-site reactions being the most common adverse event.
Conclusion
Lenacapavir is a potent, long-acting agent effective in MDR HIV and recently approved for PrEP. Its unique mechanism offers advantages in treatment and prevention. Further studies in pregnant, lactating women, and pediatric populations are needed to expand its role in preventing HIV transmission.
Abstract 019 ASPICON 2025 |September 04 -07 | 2025 |
Understanding Public and Health Care Workers Apprehension during the 2025 COVID-19 Resurgence
Harsha Suresh Mathew*, Fatima Khan
Department of Microbiology, JNMC, AMU, Aligarh, Uttar Pradesh, India.
* Presenting author: harshamathew96@gmail.com
Background
The reappearance of COVID-19 cases in 2025 has triggered renewed concern among healthcare professionals and the general population. Understanding public perception, preparedness, and associated challenges is vital for designing effective public health responses.
Objective: To assess awareness, opinions, and readiness of healthcare workers and the general community during the COVID-19 resurgence in India (2025).
Material & Methodology
A descriptive, cross-sectional study was conducted using a structured online questionnaire. Responses were collected from participants across various Indian states, covering demographics, information sources, perceived severity of the wave, preparedness levels, PPE availability, and attitudes toward booster vaccination.
Results
More than 100 participants were analyzed:
● Demographics: About 70% were from healthcare backgrounds. The remaining 30% were from the general public
● Awareness & Information: All respondents were aware of rising COVID-19 cases
Main information sources: digital media and online platforms
● Perception of Severity: Responses were mixed; many were uncertain or did not view this wave as more severe
● Vaccination & Boosters: Most acknowledged vaccine protection. Several expressed doubts regarding additional booster doses
● Preventive Practices: Most participants reported using masks and maintaining hygiene at least occasionally
● Healthcare Readiness: Many healthcare workers felt only “somewhat prepared”. Challenges included staff shortages and inadequate protective gear
● Mental Health & Concerns: Common issues: emotional fatigue, fear of lockdowns, rising cases and fear of morbidity among comorbid patients, and public noncompliance
Conclusion
The study reveals varying levels of preparedness and significant concern. Reinforcing healthcare infrastructure, improving public communication, and supporting mental health are critical to controlling future COVID-19 waves.
Keywords: COVID-19; Public awareness; Healthcare preparedness; Booster acceptance; Mental health; 2025 wave; India
Abstract 020 ASPICON 2025 |September 04 -07 | 2025 |
Bacteriological Profile of Uropathogens in Women of Reproductive Age Group
Vindhya M1*, Ramakrishna Pai Jakribettu2*, Sumit Rai2, Vasudha C L2, Mohan Kumar2, Debabrata Dash2, Nidhima Aggrawal2
1- Malabar Medical College, Kozhikode, Kerala, India.
2- Department of Microbiology, All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India
* Presenting author: Ramakrishna.paij@gmail.com
Background
Urinary tract infections (UTIs) are one of the most common community and nosocomial infections encountered by clinicians in developing countries. Nearly half of the women population experience at least 1 episode of UTI in their lifetime, with 20-40% of them exhibiting recurrent episodes. It is a common complication during pregnancy, occurring in about 8.8% of pregnant women in India. To prescribe appropriate antibiotic therapy, the physician must have the required information about the pathogen causing the infection as well as their susceptibility patterns especially oral antimicrobials when prescribed on out-patient basis.
Aims & Objectives: To determine the bacteriological profile of uropathogens among women of reproductive age group & to determine the antimicrobial resistance pattern among commonly prescribed oral antimicrobials for UTI.
Material & Methodology
It was a record based retrospective study. All women of reproductive age group, who were diagnosed with UTI and significant bacteriuria during the study period of January 2021 to December 2022. The uropathogens isolated from the samples were subjected to VITEK-2 (bioMérieux, France) for identification and antimicrobial susceptibility testing (AST). The details obtained will be entered in Microsoft Excel and were coded and statistically analysed by frequency and percentage.
Results
A total of 553 women of reproductive age group, were diagnosed with UTI during the study period. In this study, we have observed that UTI is common among the WRAG, especially at the younger age of 18-30 years. In our patients, the incidence of UTI as increased with the higher the parity of pregnancy. The common uropathogen causing UTI are E. coli and Staphylococcus sp among Gram negative and Gram-positive pathogens, respectively. The E. coli isolates are resistant to common oral AMA like Ampicillin, amoxiclav, ciprofloxacin but nitrofurantoin have been observed to have lesser resistance. The isolation rate of MRSA is high in UTI among our patients, a matter of concern, hence the clinicians should be vigilant about the MRSA causing UTI among women of reproductive age group, which in turn increases morbidity in these patients.
Conclusion
In our study women younger age i.e., 18-30 years and higher parity of pregnancy have higher risk of having UTI. The isolation of MDR gram negative pathogens, which are resistant to commonly prescribed oral AMA, is of concern.
Keywords: UTI; Women; Reproductive age; E.coli, AMR; Oral AMA
Abstract 021 ASPICON 2025 |September 04 -07 | 2025 |
Renal Mucormycosis in a Critically Ill Patient: A Lethal Sequela of Repeated Urological Instrumentation
Mudita Khattri¹*, Saumyarup Pal¹, Gaurav Karn¹, Vanya Singh2 Ravi Kant ¹
1- Department of Internal Medicine, All India Institute of Medical Sciences, Rishikesh, India
2- Department of Microbiology, All India Institute of Medical Sciences, Rishikesh, India
* Presenting author: khattrimudi@gmail.com
Background
Mucormycosis is a rare medical condition that is caused by taxonomy of Mucorales, the most common being Rhizopus arrhizius. Though immunocompromised status is considered the main predisposing factor, there have been case reports suggesting critically ill patients, especially those undergoing repeated invasive procedures, may also be susceptible. We report a case of isolated renal mucormycosis in a critically ill patient likely prompted by repeated urological interventions, highlighting the diagnostic and therapeutic dilemma faced during the management of the case due to multiple existing comorbidities.
Case History
We report a case of a female in her 50s with no prior comorbidities, who initially presented with urinary complaints, later diagnosed with urosepsis and acute renal failure secondary to bilateral obstructive hydroureteronephrosis. Despite initial management with percutaneous nephrostomy (PCN) and antibiotics, her condition deteriorated. Cultures from the drains grew Rhizopus, confirming renal mucormycosis. Treatment with liposomal amphotericin B was initiated, along with dialysis. Surgical nephrectomy was considered but was not performed due to high surgical risk. However, due to worsening sepsis, along with multiorgan dysfunction, patient scummed to death.
Discussion
Mucormycosis is a rare angio-invasive fungal infection with a substantial degree of fatality. One unique entity seen in India is the increasing prevalence of renal mucormycosis in immunocompetent hosts. The management of mucormycosis comprises early initiation of therapy, source reduction in the form of surgical debridement, antifungal therapy, and treatment of underlying comorbidity. Although PCN is a valuable therapeutic tool, its potential role in promoting infections like mucormycosis, particularly in high-risk individuals, warrants careful procedural asepsis and vigilant postoperative monitoring.
Conclusion
Thus, the case highlights significance of maintaining a high index of suspicion for mucormycosis in patients with urosepsis who have undergone multiple urological interventions and show poor response to antimicrobial therapy.
Abstract 022 ASPICON 2025 |September 04 -07 | 2025 |
A Study on Bacterial Culture and Antibiotic Sensitivity Pattern of Ear Discharge In Chronic Otitis Media
R Rama Soujanya*, Satvinder Singh Bakshi, Seepana Ramesh, Soumyajit Das, Sumit Rai
1- Dept. of Microbiology, AIIMS Mangalagiri, Andhra Pradesh, India.
* Presenting author: soujirr@gmail.com
Objective
This study aims to evaluate the Bacterial profile of micro organisms causing mucosal type, chronic otitis media and compare their Antibiotic sensitivity pattern to available antibiotics.
Material & Methodology
This retrospective clinical study was conducted over 24 months in ENT Department, AIIMS Mangalagiri. Aural swabs were collected from 221 patients clinically diagnosed with mucosal type, chronic otitis media using sterile swabs and sent for culture and sensitivity testing. Identification of organisms was done using standard microbiological techniques. Antibiotic susceptibility was tested using Kirby –Bauer disc diffusion method.
Results
Out of 221 samples, 94 % showed positive Bacterial growth. The most commonly isolated organisms were pseudomonas aeruginosa (43%), staphylococcus aureus (37%), proteus mirabilis (5%) and Escherichia coli (4 %). Pseudomonas aeruginosa showed highest sensitivity to Neosporin H and ciprofloxacin ear drops while staphylococcus aureus was most sensitive to Neosporin H. Resistance to commonly used antibiotics such as Ampicillin and cotrimoxazole was noted.
Conclusion
The bacteriological profile of chronic otitis media showed a high prevalence of pseudomonas aeruginosa, followed by staphylococcus aureus & klebsiella species with different distributions in different age groups. The study highlights the importance of culture and sensitivity testing in treating chronic otitis media.
Empirical therapy should be re-evaluated periodically to reduce Antibiotic resistance and improve clinical outcomes.
Keywards: Chronic otitis media, mucosal type, bacterial profile and antibiotic sensitivity.
Abstract 023 ASPICON 2025 |September 04 -07 | 2025 |
Prevalence of Synergy Between Ceftazidime/ Avibactam with Aztreonam among Carbapenem Resistant Gram Negative Bacilli in A Tertiary Care Hospital
Sriram Kannuri1*, Sahjid Mukhida2, Nageswari Gandham2, Shahzad Beg Mirza2
1- Department of Clinical Microbiology, AIIMS Mangalagiri, Andhra Pradesh, India.
2- Department of Microbiology, Dr D Y Patil Medical College, Pune, Maharastra, India.
* Presenting author: ksr27081993@gmail.com
Introduction
Since the introduction of antibiotics, the emergence of microbial resistance was inevitable. Despite the availability of a variety of antibiotics, resistance to multiple types has quickly become prevalent. Carbapenems and polymyxins are commonly viewed as the final line of defense. With carbapenem resistance on the rise and colistin’s usage limited due to its toxicity, the combination of ceftazidime/avibactam (CZA) has been adopted as an alternative to colistin. However, the efficacy of CZA is constrained. Aztreonam (ATM) is used to treat specific Gram-negative infections resistant to other medications but its use is restricted; when paired with CZA, its effectiveness broadens. Nonetheless, instances of treatment failures have been observed with the CZA–ATM combination. This study investigates failure of synergy with in-vitro tests, emphasising the need for strategies to combat drug resistant pathogens.
Material & Methodology
Cross-sectional observational study conducted at Dr D Y Patil Medical College, Pune between 1st April 2022 and 30th June 2022. Processed 444 among which 87 Carbapenem Resistant Enterobacterales and Carbapenem Resistant Pseudomonas aeruginosa resistant to CZA and ATM, were included in the study and subjected to synergy by stacking CZA and ATM E-test strips on MHA with test organism lawn. Data analyzed using excel.
Results
87 isolates, 61 Klebsiella pneumoniae(Kpn), 21 Escherichia coli(Eco) and 5 Pseudomonas aeruginosa(Pae). Of isolates tested for synergy 5 showed no synergy, 3 Kpn, 1 Eco and 1 Pae, Kpn was isolated from pus and blood, Eco from peritoneal fluid, Pae from pus.
Conclusion
The combination works, but the instances where the synergy fails and this failure which is insignificant now will surely rise exponentially in future. We have to be mindful of this and are in urgent need of newer antibiotics or combinations. As a first step towards a brighter future, it isimperative to use antibiotics judiciously and practice antibiotic holiday.
Abstract 024 ASPICON 2025 |September 04 -07 | 2025 |
Cerberus Otitis- Acinetobacter Baumannii-Mediated Fulminant Otitis Media
Hari Haran .G*, Mounika.A, T. Prathyusha, U.K.Rakesh, K. V. Sharada
Department of Medicine, All India Institute of Medical Sciences,Mangalagiri,AndhraPradesh, India.
* Presenting author: rajihari865@gmail.com
Background
Carbapenem-Resistant Acinetobacter baumannii (CRAB) is a formidable nosocomial pathogen, particularly within the intensive care unit (ICU). While commonly associated with ventilator-associated pneumonia and bloodstream infections, its role as a primary pathogen in otogenic sepsis is exceptionally rare and portends a challenging clinical course due to extensive multidrug resistance.
Aim & Objectives: Our Aim is to present a case of AOM in an ICU patient with ear swab culture positive for CRAB and discuss clinical management and outcomes.
Case Presentation
We present the case of an adult patient admitted to the medical ICU who developed acute otitis media (AOM) secondary to CRAB, identified via swab culture. The infection occurred in the context of immunocompromised ,multisystemic infection. This otogenic focus was subsequently implicated as a likely source of occult sepsis, complicating the patient’s management.
Patient developed acute onset severe excruciating earache and ear fullness and sudden onset hearing loss with pus discharge.otoscopy finding show perforation ,congested tympanic membrane with pus discharge.Swab culture sensitivity reveals CRAB +ve with resistance to multiple drugs.patient was initiated immediately on Injection polymixin B and minocycline with colistin .patient started showing clinical improvement with resolution of the pus discharge and restoration of hearing.
Interpretation: This case illustrates a novel and severe manifestation of CRAB infection, which we propose under the colloquial designation “Cerberus Otitis” to reflect its multidrug-resistant (MDR), multi-headed challenges and dire prognosis. It underscores the necessity for meticulous otologic examination in septic ICU patients and reinforces the critical importance of antimicrobial stewardship and infection control protocols to mitigate the spread of such pan-resistant organisms in high-acuity settings.
Conclusion
This case highlights the importance of microbiological evaluation in ICU patients with AOM and the challenge posed by CRAB. Early detection and tailored antibiotic treatment are critical for successful management.
Keywords: Acinetobacter baumannii; Carbapenem-Resistant; Nosocomial Infection; Otitis Media; Intensive Care Units; Sepsis; Multidrug Resistance.
Abstract 025 ASPICON 2025 |September 04 -07 | 2025 |
A Community based Cross-sectional Study to Assess the Prevalence, Knowledge and Practices of Self-Medication of Antibiotics
Sathiyanarayanan S*, Rajeev A, Kalaiselvan G, Rashmitha P, Subitsha, Vijay Kishore, Ravi
Department of Community and Family Medicine, All India Institute of Medical Sciences,Mangalagiri,AndhraPradesh, India.
* Presenting author: sathiya@aiimsmangalagiri.edu.in
Background
Self-medication with antibiotics is a growing public health concern, contributing significantly to the emergence of antimicrobial resistance (AMR). Inappropriate use of antibiotics without prescription remains prevalent in developing countries due to easy over-the-counter access, lack of awareness, and poor regulatory control.
Objectives: To assess the prevalence, knowledge, and practices related to self-medication with antibiotics among adult residents of Mangalagiri town and evaluate the impact of a structured health education intervention.
Material & Methodology
A community-based cross-sectional study was conducted over six months among 482 adults aged 18–65 years in Mangalagiri, Andhra Pradesh using stratified random sampling. Data were collected using a validated, structured questionnaire, assessing prior antibiotic self-medication, knowledge, and practices. A 15-minute health education intervention was delivered to all participants, followed by a post-intervention knowledge assessment.
Result
Among 482 participants, 63.9% were males and 36.1% were females with the mean age of 42.34 +/-14.51. A greater number of males were in the highest income category and conversely lower income brackets had a disproportionately higher number of female participants, suggesting an economic vulnerability among women. When had any need of medication, 36.9% of participants consulted a doctor, while 35.3% of participants bought antibiotics from a pharmacy, 19.9% of participants used leftover antibiotics with them, and 7.9% participants asked a friend for advice. The mean knowledge score increased from 4.00 to 9.16 (p-value <0.001) after the intervention. The participants with lower educational levels demonstrated the highest gains in knowledge scores and participants with higher education showed less improvement, possibly due to already having better baseline knowledge prior to the intervention.
Conclusion
The study highlights a high prevalence of self-medication with antibiotics and limited baseline knowledge among the community. The significant improvement in post-intervention knowledge scores, particularly among participants with lower educational status, demonstrates the effectiveness of targeted health education.
Abstract 026 ASPICON 2025 |September 04 -07 | 2025 |
One and half -Year Retrospective Data Analysis of Pyelonephritis Presentation and Management: Opportunities for Stewardship Intervention to prevent Drug overuse and Complications
T. Prathyusha*, R. Nanda Kishore, K Shanmukh Krishna, A. Gowtham, M. Rajendra Prasad
Department of Medicine, All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India.
* Presenting author: prathyu.9@aiimsmangalagiri.edu.in
Background
Pyelonephritis represents a high-burden condition with significant implications for antimicrobial resistance (AMR) and resource utilization. Despite established guidelines (IDSA/EUA), suboptimal management practices, including inappropriate broad-spectrum antibiotic use and delayed IV-to-oral transition, are frequently reported. Antimicrobial Stewardship Programs (ASPs) require institution-specific data to design effective interventions for preventing drug resistance ,cost effectiveness and drug long term side-effects
Aims & Objectives:
1. Assess adherence to key IDSA/ESCMID 2025 guideline recommendations for pyelonephritis management.
2. Quantify specific stewardship opportunity areas (e.g., inappropriate fluoroquinolone use, prolonged IV duration, excessive total treatment length,drug longtermsideeffects)
3. Quantify clinical outcomes (30-day readmission, treatment failure) by antibiotic regimen4.Assess the pattern of cultures growth and assess senstive /resistant antibiotics to establish a local antibiogram and stream line regular audits in the institute
Material & Methodology
A retrospective pilot study was conducted in aiims mangalagiri, reviewing electronic health records of adult patients diagnosed with pyelonephritis between 01-01-2024 and 31-07-2025. Data extraction was focused on patient demographics, risk factors, illness severity, empiric and definitive antibiotic therapy (spectrum, agent), timing of IV-to-oral transition, total treatment duration, and adherence to IDSA/EUA guidelines, culture results, antibiotic sensitivity and resistance patterns and clinical outcomes (length of stay, treatment failure, C. difficile infection, 30-day readmission).
Result
A total of 72 patients were included in the data analysis. The cohort was 75% female and 25% male. Overall adherence to empirical antibiotic initiation was high at 98%. However, the median time to switch from intravenous to oral antibiotic therapy was 10 days, which is non-compliant with standard guidelines. The median hospital stay was 15 days.The all-cause readmission rate was 6%, primarily attributed to uncontrolled diabetes and other comorbidities. Due to prolonged antibiotic administration, the rate of Clostridium difficile infection was 6%.
Culture-positive results were obtained in 70% of cases, with E. coli and Klebsiella species being the predominant pathogens. The majority of these isolates were sensitive to Piperacillin-Tazobactam and Meropenem. Notably, a 5% incidence of Carbapenem-Resistant Acinetobacter baumannii (CRAB) positive growth was observed, which presented a significant challenge for further management.
Conclusion
Based on these findings, it is concluded that while empirical antibiotic initiation for pyelonephritis was highly adherent and effective against the predominant pathogens E. coli and Klebsiella, a significant delay in intravenous-to-oral switch contributed to prolonged hospitalization and a 6% rate of C. difficile infection. The 6% readmission rate, driven by comorbidities, and the emergence of challenging Carbapenem-Resistant Acinetobacter baumannii (5%) underscore the critical need for antimicrobial stewardship to optimize therapy transitions and vigilant monitoring to manage resistant organisms.
Abstract 027 ASPICON 2025 |September 04 -07 | 2025 |
A Systematic Review on Innovative Approaches to Antimicrobial Stewardship Strategies, Technologies and Clinical Effectiveness
Sarikonda Sandhya Rani1*, L V Simhachalam Kutikuppala2, CL Vasudha1, Sushil Sharma1, Madhavrao C1, Arup Kumar Misra1
1- All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India.
2- Rajshree Medical Research Institute, Bareilly, Uttar Pradesh, India.
* Presenting author: sandhyapharm89@gmail.com
Background
Antimicrobial resistance (AMR) remains a pressing challenge for health systems worldwide, undermining the effectiveness of routine treatments. In response, antimicrobial stewardship (AMS) programs have evolved to incorporate digital tools and novel strategies aimed at improving prescribing practices.
Aims & Objectives: To explore the range of innovative AMS interventions and assesses their impact on clinical outcomes, antibiotic use, and implementation feasibility.
Material & Methodology
A comprehensive literature search was conducted across six major databases: PubMed, Embase, the Cochrane Library, Scopus, Web of Science, and CINAHL up to July 2025. Eligible studies included various study designs from randomized controlled trials to qualitative studies focusing on AMS interventions using technology or novel frameworks. Two reviewers independently screened and extracted the data. Risk of bias was assessed using established tools including RoB 2.0, ROBINS-I and CASP. Data were synthesized using a structured narrative approach, pooling up the findings in terms of intervention type, healthcare setting and reported outcomes.
Result
Out of 6,481 screened records, 72 studies met the inclusion criteria. The interventions examined included electronic prescribing systems, AI-powered decision support, mobile health apps and telehealth-enabled AMS programs. Most studies reported reductions in inappropriate antibiotic prescribing and improvements in adherence to clinical guidelines. Some also demonstrated favorable trends in resistance patterns and patient outcomes. Implementation success varied, often influenced by infrastructure, clinical workflow integration, and user engagement. Cost-effectiveness data, though limited, suggested potential financial benefits, particularly for digitally supported programs.
Conclusion
Emerging technologies and strategic innovations in AMS show considerable promise in optimizing antibiotic use and enhancing patient care. Their success largely depends on local implementation contexts and resource availability. Further rigorous studies, especially in low-resource settings, are needed to strengthen the evidence-based strategies in guiding policy and practice.
Abstract 028 ASPICON 2025 |September 04 -07 | 2025 |
Evaluation of a novel method for Determination of Vancomycin MIC’s in Staphylococcus aureus and its Comparison with an In- house Agar Gradient Test
Priyadharshanni A*, Nidhima Aggarwal, Sumit Rai, Debabrata Dash
All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India.
* Presenting author: priyadharshanni@gmail.com
Background
Staphylococcus aureus, is one of the commonest aetiologies of skin and soft tissues infections, bacteraemia, sepsis, osteoarthritis, food poisoning and community acquired pneumonias. It is well known for its notoriety in developing resistance against various drugs, especially in the MRSA isolates, which form a significant percentage among these infections. The MRSA prevalence has risen from 23% to 30% from 2022 to 2024 at AIIMS Mangalagiri. The ICMR 2023 data highlights a national prevalence from the participating labs as 44.5%. Vancomycin is the drug of choice for targeted therapy against MRSA, for which vancomycin needs to be tested by only by MIC determination protocols especially to detect Vancomycin-intermediate S. aureus (VISA) and heterogeneous VISA (hVISA) phenotype. Current MIC determination methods for vancomycin commonly include automated methods, which may be expensive or not commonly available. The commercial agar gradient E-test strips, which are expensive and both are marred by supply chain issues. The gold standard method broth microdilution is not routinely performed in most of the diagnostic labs as it is cumbersome and technically challenging.
With this premise, a new method Vancomycin broth disk elution (VBDE) method similar to Colistin Broth Disk Elution method was assessed in this study and it was assessed alongside the in – house developed Agar Gradient Test.
Aims & Objectives: To develop, optimize and standardize the VBDE method and validate it against the BMD Reference Method for determination of Vancomycin MIC in Staphylococcus aureus isolates from various clinical specimens.
To compare the VBDE with the standardized in – house developed Agar Gradient Test
Material & Methodology
A pilot prospective cross- sectional analytical study was conducted with non-repeat strains of Staphylococcus aureus isolated from different clinical specimens over a period of 3 months duration were included in the study. Isolates were designated MSSA or MRSA based on susceptibility to Cefoxitin in Kirby-Bauer disk diffusion method as per CLSI guidelines. They were subjected to MIC determination by novel disk elution method VBDE and gold standard BMD in addition to routine Antimicrobial Susceptibility Testing (AST). These isolates were also subjected to the in – house developed Agar Gradient Test
Result
All isolates tested were susceptible to Vancomycin with range of MIC from 1µg/ml to 2µg/ml. Using BMD as reference, the novel method VBDE demonstrated sensitivity and specificity of more than 90%. And the level of agreement in measuring MIC between BMD and VBDE was assessed using Intraclass correlation coefficient (Two-way random effect, absolute agreement formula) shows high agreement (>0.9) with confidence interval of 95%.
Conclusion
The VBDE protocol is a novel, reproducible method that can be used in routine diagnostic laboratories to report vancomycin MIC values for MRSA Isolates.
Abstract 029 ASPICON 2025 |September 04 -07 | 2025 |
Effect of Empirical Gram-Positive and Gram-Negative Antibiotic Coverage on Mortality and Recovery in Sepsis: Interim Results from a Prospective Cohort Study
Bharath Kumar G*, Bikash Ranjan Meher, Biswa Mohan Padhy, Rasmi Ranjan Mohanty, Srikant Bhara
All India Institute of Medical Sciences, Bhubaneswar, Odisha, India
* Presenting author: bharathkumarg24@gmail.com
Introduction
Sepsis continues to be a major cause of mortality worldwide. Early empirical antimicrobial therapy is a cornerstone of sepsis management, yet there is a lack of consensus in India regarding the inclusion of gram-positive coverage. This study evaluates whether empirical therapy combining gram-positive and gram-negative agents improves clinical outcomes compared to gram-negative coverage alone.
Objectives:
To compare in-hospital mortality between two empirical antimicrobial strategies:
1. Gram-negative coverage only (G−)
2. Combined gram-positive and gram-negative coverage (G+G−)
Secondary objectives include comparing hospital stay duration, CRP/PCT/WBC/neutrophil trends.
Material & Methodology
This is an ongoing prospective cohort study conducted at a tertiary care center. Adult patients (≥18 years) with sepsis or septic shock were enrolled. Patients were grouped based on empirical therapy received. This interim analysis includes 56 patients. The primary outcome was in-hospital mortality. Secondary outcomes included length of hospital stay (analysed only in survivors) and changes in biomarkers. Mortality was assessed using Chi-square test. Length of stay was compared using Wilcoxon rank-sum test. Biomarker outcomes were analysed using ANCOVA models adjusted for baseline values.
Result
In-hospital mortality was significantly lower in the G+G− group (18%) compared to the G− group (86%) (χ² = 23.17, p < 0.0001). Among survivors, the median length of stay was significantly shorter in the G+G− group (20 days, IQR: 14) than G− group (53.5 days, IQR: 18) (p = 0.0069). ANCOVA showed significantly greater reduction in CRP (β = 47.86, p < 0.0001), PCT (β = 9.29, p = 0.0015), WBC (β = 10.92, p < 0.0001), and neutrophil percentage (β = 25.83, p < 0.0001) in the G+G− group.
Conclusion
This interim analysis suggests that empirical antibiotic coverage including gram-positive agents may lead to lower mortality, shorter hospital stay, and faster biomarker resolution in sepsis.
Abstract 030 ASPICON 2025 |September 04 -07 | 2025 |
Characterization of Carbapenem-Resistant Gram-Negative Bacteria (CR-GNB) from ICU Patients Using Molecular and Phenotypic Methods.
Aishwarya D.Warang*, Sharvari A.Samant, Sagar Sinha
MGM Medical College, Kamothe, MGMIHS, Navi Mumbai, India.
* Presenting author: warangaish8@gmail.com
Introduction
Carbapenem-Resistant Gram-negative bacteria (CR-GNB) are a major cause of ICU infections and public health concern. Resistance is often due to metallo-β-lactamases (MBL) like NDM, encoded by the bla NDM-1 gene, which hydrolyze β-lactam antibiotics. This study aims to characterize CR-GNB from ICU patients using phenotypic and molecular methods.
Objectives:
1. To isolate and characterize CR-GNB from ICU patients.
2. Phenotypic detection of MBL production in CR-GNB.
3. Genotypic Detection of bla NDM -1 by PCR in CR-GNB
Material & Methodology
A total of 200 clinical isolates were collected from ICU patients. Carbapenem resistance was screened using the Kirby-Bauer disc diffusion method as per CLSI guidelines. MBL production was detected by performing Modified Hodge Test (MHT), Double Disc Synergy Test (DDST) and Combined Disc Synergy Test (CDST). The bla NDM-1 genes were detected by Polymerase Chain Reaction (PCR).
Result
Out of 911 GNB isolated from ICU patients, 200 isolates (22%) were identified as CR-GNB. The most predominant organism was Enterobacter spp 47 (23.5%) followed by Acinetobacter spp 44 (22 %) Klebsiella spp 40 (20% ), E.coli 30 (15 %), Pseudomonas spp 29 (14.5 %), Proteus spp 5 (2.5%) , Citrobacter spp 5 (2.5%). (5, 2.5%). All 200 CR-GNB isolates were subjected to phenotypic testing by Modified Hodge Test (MHT), Double Disc Synergy Test (DDST), and Combined Disc Synergy Test (CDST), and PCR was performed to detect the bla NDM-1 gene. The bla NDM-1 gene was detected in Proteus spp 5/5 (100%), Klebsiella spp 30/40 (75%), Acinetobacter spp 32/44 (73 %), Enterobacter spp 34/47(72%) , E.coli 20/30 (67 %) , Citrobacter spp 3/5(60%), Pseudomonas spp 15/29 (52 %).
Conclusion
Out of 200 CR-GNB isolates, MBL production was detected in 148 isolates by CDST, which was more sensitive than MHT and DDST. The bla NDM-1 gene was identified in 139 isolates. The isolates lacking bla NDM-1 gene, resistance may be due to other genes. CDST can partially substitute PCR for CR-GNB detection in resource-limited or outbreak settings.
Keywords: Carbapenem; Modified Hodge Test; Double Disc Synergy Test; Combined Disc Synergy Test.
Abstract 031 ASPICON 2025 |September 04 -07 | 2025 |
A Systematic Review on Global Resilience of Antimicrobial Stewardship Programs during COVID-19: Disruptions and Innovations
Vennela Jyothi*, Madhavrao C, Sushil Sharma, Gaurav M Rangari, Arup Kumar Misra, Srinivasa Rao K
Department of Pharmacology, All India Institute Of Medical Sciences (AIIMS), Mangalagiri, India.
* Presenting author: jyothivennela9@gmail.com
Introduction
The COVID-19 pandemic significantly disrupted healthcare systems worldwide, including routine antimicrobial stewardship (ASPs) programs. The crisis led to widespread empirical antibiotic prescribing despite low bacterial co-infection rates, exacerbating concerns about antimicrobial resistance (AMR). Understanding how ASPs evolved during this period is crucial for developing effective pandemic preparedness strategies for the future.
Aims & Objectives: To systematically review the global impact of COVID-19 on ASPs, with a dual focus on (1) disruptions to stewardship activities and (2) adaptive strategies or innovations implemented to maintain ASP functions during the pandemic.
Material & Methodology
A comprehensive search strategy has been designed to identify relevant studies published between January 2020 and April 2024 from PubMed, Embase, Scopus, and Web of Science. Articles were included if they described disruptions, adaptations, or innovations in hospital-based ASPs during the pandemic. The PRISMA 2020 guidelines were followed, and the risk of bias was assessed using the Newcastle-Ottawa Scale and ROBINS-I tools.
Result
Out of 2,417 articles screened, 67 studies from 24 countries met the inclusion criteria.
Interruptions included increased use of empirical antibiotics (78%), restricted access to microbiology labs (47%), and diversion of ASP staff to COVID-19 care (63%). However, 52% of studies reported digital adaptations, including tele-stewardship, electronic decision tools, and automated alerts. Strategies included multidisciplinary collaboration, national policy support, and the integration of ASPs into pandemic preparedness frameworks. Innovations like AI-driven infection prediction and e-learning platforms for AMS training were also highlighted.
Conclusion
COVID-19 challenged the continuity of ASPs, but simultaneously accelerated digital transformation and policy innovation. Integrating technology, flexible staffing models, and proactive leadership were pivotal in sustaining stewardship activities. The insights offered guidance for strengthening ASP’s resilience in future health crises.
Abstract 032 ASPICON 2025 |September 04 -07 | 2025 |
Impact of Artificial Intelligence versus Conventional Approaches in Antimicrobial Stewardship: A Systematic Review
Hemanth Kumar*, Sushil Sharma, Madhavrao C, Gaurav Manikrao Rangari, Arup Kumar Misra, Srinivasa Rao Katiboina
Department of Pharmacology, All India Institute Of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India.
* Presenting author: jyothivennela9@gmail.com
Background
Antimicrobial resistance (AMR) is a significant global health threat, driven largely by the inappropriate use of antibiotics. Antimicrobial Stewardship Programs (AMS) are crucial for optimizing antimicrobial use, but traditional methods like manual prescription reviews are resource-intensive. Artificial intelligence (AI)-based Clinical Decision Support Systems (CDSS) may enhance stewardship by predicting infections and guiding appropriate.
Aims & Objectives: The primary aim of this study is to systematically review and compare the predictive performance of AI/ML models with conventional statistical approaches. The objectives are to assess whether AI-powered tools improve the accuracy of antimicrobial prescribing decisions and evaluate if AI models can more effectively predict bloodstream infections and culture results compared to traditional methods.
Material & Methodology
A systematic literature search was conducted in PubMed/MEDLINE, Scopus and EMBASE up to July 2024. Studies were included if they directly compared the performance of an AI/ML model to a traditional statistical model for an AMS-related outcome. Data on study design, patient populations, and model performance metrics—including Area Under the Curve (AUC), accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV)—were extracted. The risk of bias was assessed using the QUADAS-AI tool. Due to significant heterogeneity, a narrative synthesis was performed.
Result
AI/ML models, particularly ensemble methods like Random Forest and Gradient Boosting, frequently demonstrated superior or comparable performance to logistic regression. For predicting bloodstream infections, AI models achieved AUCs as high as 0.88, outperforming logistic regression (AUCs up to 0.86). AI models consistently showed higher sensitivity and NPV across various applications, indicating a stronger ability to correctly identify high-risk patients and reliably rule out infections. However, specificity was more variable, with logistic regression sometimes performing comparably. A universal lack of external validation was a key limitation across all studies.
Conclusion
AI-powered CDSS consistently outperform conventional approaches in optimizing antimicrobial prescribing, predicting infections, and forecasting resistance. These tools show promise for reducing inappropriate antibiotic use and strengthening ASPs, though external validation and real-world integration remain necessary before widespread adoption.
Abstract 033 ASPICON 2025 |September 04 -07 | 2025 |
Isolation of Dermatphytes in Chronic and Recurrent Dermatophytosis Cases in a Teaching Care Hospital
Manasa Sireesha Devara*, Matta Harika Priya, Vijaya Bharathi D
Gayatri Vidya Parishad Institute of Health Care and Medical Technology(GVPIHC&MT), Visakhapatnam,Andhra Pradesh, India.
* Presenting author: devaramanasa18@gmail.com
Background
Dermatophytosis, which affects millions of individuals globally, is one of the most prevalent superficial skin diseases.It has been determined that 20% to 25% of the global population has superficial mycoses, with a higher prevalence in tropical and subtropical nations like India. The most common organism in India, according to recent studies, is Trichophyton rubrum. However, Trichophyton mentagrophytes is now the co-dominant pathogen . This shift in the epidemiology of dermatophytes may be the cause of persistent, recurrent, and resistant cases of dermatophytosis.
Aims & Objective: To determine the mycological profile of chronic and recurrent dermatophytic infections, including species identification.
Material & Methodology
The present study includes a total of 75 chronic and reccurent dermatopytosis patients who are attending to Dermatology department of our hospital. The specimens skin scrapings,hair, scraping of the nails was examined under a microscope using 10%&40% KOH to look for presence of hyphae in skin,hair and nails. The collected specimens inoculated and incubated at 28⁰C for 4 weeks by using Dermatophyte test media and Sabarouds dextrose agar.Later the growth of the isolate were examined.
Result
In the present study, out of 75 cases maximum patients were reported in the age group of 18-30 years [40%]. According to this study, Males (56%) were more affected than female(44%) and topical corticosteroids application(17.3%) was the most common predisposing factor. The most common clinical presentation observed was Tinea corporis et cruris patients (41.3%) and
Trichophyton mentagrophytes was isolated in 27 cases, making it was the most common isolate (36%), followed by Trichophyton verrucosum in 12 cases (16 %),Trichophyton tonsurans in 10 cases (13.3%) and other isolates in the present study.
Conclusion
To conclude, reccurent and chronic dermatophytosis could be reduced and prevented by health educating the patients and also by isolation dermatophytes for specific treatment.
Keywords: Dermatophytes,Topical steroids; Chronic and Reccurent dermatophytosis.
Abstract 034 ASPICON 2025 |September 04 -07 | 2025 |
Assessment of Antimicrobial Use in the Emergency Services: A Retrospective Audit Based on Risk Stratification and WHO AWaRe Classification
Jovita Davis Chirame*, Aruna Poojary, Priyanka Patil
Breach Candy Hospital Trust Mumbai, Maharashtra, India.
* Presenting author: dr.jovitadavis@gmail.com
Background
Emergency Medical Services (EMS) serve as critical transition points between community and hospital care. Due to time constraints and clinical urgency, empirical antimicrobial prescribing is common, increasing the risk of inappropriate use. The WHO AWaRe framework recommends that ≥60% of antibiotics used belong to the Access group to help mitigate antimicrobial resistance.
Aims & Objectives: To evaluate antimicrobial prescribing patterns in the EMS, correlate them with presenting syndromes and risk stratification, and classify agents according to the WHO AWaRe framework.
Material & Methodology
A retrospective audit was conducted from 1st–31st May 2025 in the EMS. Medical records of all patients during this period were reviewed. Those receiving at least one antimicrobial were included. Data on demographics, clinical syndrome, diagnosis, and antimicrobials prescribed were analyzed per WHO AWaRe categories and risk stratification.
Result
Among 886 patients, 69% were discharged and 31% admitted. Overall, 24% received antimicrobials—21% of discharged and 32% of admitted patients. Discharged patients receiving AMAs were mostly low-risk (79% Type 1), while admitted patients were predominantly high-risk (56% Type 3). AMA use was highest among 18–40-year-olds (discharged) and those >60 years (admitted). Females constituted 54% of AMA recipients. Fever, GI disorders, and respiratory infections were the most common indications. According to AWaRe classification, 43% of prescribed AMAs were Access, 51% Watch, and 2% Reserve. Irrational combinations were noted in 2% of cases.
Conclusion
Antimicrobial use in EMS reflects a high reliance on Watch group agents and suboptimal adherence to AWaRe targets. The presence of irrational combinations and higher-risk prescribing in admitted patients highlights the need for improved stewardship strategies. Strengthening syndrome-based protocols, promoting rational empirical use, and aligning practices with AWaRe guidelines are critical to ensure appropriate antimicrobial use and reduce the risk of resistance in this fast-paced clinical setting.
Abstract 035 ASPICON 2025 |September 04 -07 | 2025 |
Comparative Analysis of Direct Antimicrobial Susceptibility Testing and Antibiotic Susceptibility Testing of Blood Cultures of Gram-Negative Organisms in a Tertiary Care Hospital
Parandhaman A*, Debabrata Dash
Department of Microbiology, All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India.
* Presenting author: aruparand@gmail.com
Background
Sepsis requires prompt diagnosis for effective management. Standard Antimicrobial Susceptibility Testing (AST) is time-consuming, highlighting the need for Direct Antimicrobial Susceptibility Testing (DST) to provide reports earlier.
Aims & Objectives: To compare the results of DST and AST in order to determine the feasibility and reliability of DST
Material & Methodology
We performed a retrospective cross-sectional comparative study conducted for 12 months at a tertiary care facility analysed positive blood culture isolates. The bottles were removed from the automated system once the sound signal of the instrument indicated the growth of bacteria, and 2 ml of broth was used for smear preparation and Gram staining, along with the microorganism identification test and DST. Only the samples containing gram-negative bacilli (GNB) were included in the study. Blood cultures with two or more morphological types, yeasts, or gram-positive organisms were excluded from the analysis.
Positive blood culture broth samples were plated on MacConkey Agar, Blood Agar and incubated at 35°C overnight to obtain isolated colonies. Routine biochemical tests were performed to identify microorganisms. The colonies were simultaneously inoculated in Mueller-Hinton Broth, making the suspension equivalent to a 0.5 McFarland standard, and then AST was performed by the Kirby-Bauer disc diffusion method. Interpretation of results was done according to the CLSI guidelines. Results were expressed in Whenever a test method yielded same susceptibility category as that of reference method, it is said to be categorically agreed. The categorical disagreement was further characterized into minor error (mE), major error (ME), and very major error (VME). When result in one method is intermediate and other method is susceptible or resistant, it is said to be mE. When reference method yields resistant category and test method yields susceptible category, this is called as very ME. When reference method result is susceptible and test method result is resistant, it is said to be ME.
Result
Assessment of categorical Agreement and disagreement was done. Pseudomonas aeruginosa has better agreement than Enterobacterales and least agreement was seen in Acinetobacter
Abstract 036 ASPICON 2025 |September 04 -07 | 2025 |
The Final Frontier of Antibiotics: Retrospective Mapping of Resistance, Utilization, and Survival in ICU Patients Battling Multidrug-Resistant Infections
Akhila Chagalamari*, Debabrata Dash, Uppara Kadiyala Rakesh, Madhavrao C, Gaurav M. Rangari, Arup Kumar Misra
All India Institute of Medical Sciences (AIIMS), Mangalagiri, Andhra Pradesh, India.
* Presenting author: akhilachagalamari03@gmail.com
Background
Multidrug-resistant (MDR) infections are increasingly prevalent in ICUs, complicating empirical antimicrobial choices. Antimicrobial resistance surveillance through antibiograms and outcome analysis is vital to guide stewardship.
Aims and Objectives: To analyse empirical antimicrobial use, resistance trends, and clinical outcomes in ICU patients with MDR infections and assess concordance with the antibiogram data.
Material & Methodology
A single-centre retrospective study was conducted at tertiary centre (Jan 2023–Nov 2024), including critically ill adult patients diagnosed with MDR infections. Data on antimicrobial use, resistance profiles, and clinical outcomes (mortality, ICU stay) were extracted from records and compared against institutional antibiogram trends. The comparison between appropriate vs inappropriate empirical therapy was analysed by using appropriate statistical tests. The P-value <0.05 was considered as statistically significant.
Result
Among ICU isolates, MRSA accounted for 46.7% of S. aureus pyogenic infections, while 7.1% of Enterococcus faecalis urine isolates were vancomycin-resistant. Blood isolates of Enterobacterales showed 86.5% susceptibility to carbapenems and 76.9% to piperacillin-tazobactam. Respiratory isolates like A. baumannii and K. pneumoniae had poor susceptibility (<70%), reinforcing the need for tailored regimens. Early appropriate empirical therapy significantly reduced mortality and ICU stay (P<0.05). Inappropriate therapy and delays were associated with poorer outcomes. Antibiotic de-escalation based on culture results showed no increase in mortality and contributed to reduced resistance burden.
In ICU isolates, A. baumannii and K. pneumoniae showed extensive drug resistance, with 0% carbapenem sensitivity; colistin remained 100% effective in both. Minocycline and cefiderocol were effective against A. baumannii, while aztreonam–avibactam was preferred in suspected NDM-producing Klebsiella. Enterococcus spp. showed 7.1% VRE, with vancomycin effective in 92.9% of cases. Fluoroquinolones were largely ineffective across organisms, underscoring the need for tailored, antibiogram-driven empirical therapy.
Conclusions
Empirical antibiotic strategies informed by local antibiogram trend improves outcome in critically ill MDR-infected patients. Continuous resistance surveillance and stewardship-driven de-escalation are critical to optimizing ICU antimicrobial protocols and combating AMR.
Keywords: Antimicrobial stewardship; ICU; multidrug resistance; antibiogram; empirical therapy; de-escalation, India
Abstract 037 ASPICON 2025 |September 04 -07 | 2025 |
Comparative Efficacy and Safety of Itraconazole, SUBA-Itraconazole, and Voriconazole in Recalcitrant Dermatophytosis: A Randomized Open label active comparator clinical Trial
Mahesh Kumar B*, Nusrat Shafiq, Sunil Dogra, Tarun Narang, Shivaprakash MR, Nikhil Aravind, Samir Malhotra, Ashish Kakkar, Biman Saikia
Postgraduate Institute of Medical Education and Research, Chandigarh, India.
* Presenting author: maheshiva.feb16@gmail.com
Background
Recalcitrant dermatophytosis poses a significant therapeutic challenge in India, driven by emerging antifungal resistance and suboptimal outcomes despite prolonged therapy. Itraconazole remains the standard of care, with recent guidelines supporting the use of SUBA-itraconazole for improved bioavailability. While early evidence suggests a potential role for voriconazole, direct head-to-head comparisons among these agents are lacking, underscoring the need for well-designed trials to guide optimal treatment strategies.
Objectives: To evaluate and compare the clinical efficacy, safety, pharmacokinetics, dermatokinetics, and immunomodulatory effects (IgE levels) of itraconazole, SUBA-itraconazole, and voriconazole in patients with recalcitrant dermatophytosis.
Material & Methodology
This prospective, randomized, open-label trial enrolled 45 patients with recalcitrant dermatophytosis, randomized equally into three parallel arms (n = 15 each) receiving itraconazole 200 mg OD, SUBA-itraconazole 130 mg OD, or voriconazole 400 mg OD for 8 weeks. Clinical cure was assessed using a composite Total Symptom Score (TSS), while mycological cure was determined via direct KOH mount. Skin scrapings were also collected for fungal culture and antifungal susceptibility testing (AFST). Serum IgE levels was measured at baseline and end of therapy. Both intention-to-treat and per-protocol analyses were performed, with safety monitored through serial organ function tests and adverse event reporting.
Result
Complete cure rates were 53.8%, 75%, and 84.6% (per-protocol), and 60%, 60%, and 73.3% (ITT) for itraconazole, SUBA-itraconazole, and voriconazole, respectively; differences were not statistically significant. Clinical and mycological cure rates followed a similar pattern, with no statistically significant differences. Relapse within 3 months occurred in 28.5% (itraconazole), 22.2% (SUBA-itraconazole), and 18.2% (voriconazole) of cured patients (p=0.875). Of the 45 enrolled patients, dermatophyte cultures were positive in 32 cases, with the Trichophyton mentagrophytes/interdigitale complex identified as the predominant species. Antifungal susceptibility testing revealed elevated minimum inhibitory concentrations (MICs) for terbinafine in the majority of isolates, whereas MICs for itraconazole and voriconazole were uniformly low (<1 µg/mL), indicating preserved in vitro susceptibility. A decline in total IgE levels was observed in all arms. Adverse events were more frequently reported in the Voriconazole group, including transient elevations in liver enzymes and visual disturbances; however, no serious adverse events or deaths occurred in any group.
Conclusions
Voriconazole demonstrated numerically higher cure rates, suggesting its potential role in recalcitrant dermatophytosis.
Keywords
Recalcitrant Dermatophytosis, Itraconazole, SUBA-Itraconazole, Voriconazole, Immunomodulation, IgE.
Abstract 038 ASPICON 2025 |September 04 -07 | 2025 |
Clinical And Antimicrobial Stewardship Impact of Matrix Assisted Laser Desorption Ionisation Time of Flight Mass Spectrometry (MALDI –TOF MS) in Blood Stream Infection Diagnostics: A Retrospective Analysis from A Quaternary Care Center in Chennai, India.
Iswarya M*, Subha S, Vidyalakshmi Devarajan, Satya, Ravi, Akila
Rela Hospital – Multispeciality Hospital in Chennai, India.
* Presenting author: ishwarya.mariappan@gmail.com
Introduction
Blood stream infections (BSI) are associated with high morbidity and mortality and hence rapid identification of pathogens is pivotal for timely targeted antimicrobial therapy. Each hour of delay in antimicrobial administration was associated with an average decrease in survival of 7.6%.Conventional methods like biochemical tests often require 48-72hrs to yield species level identification, delaying definitive clinical decisions. MALDI-TOF MS offers rapid and species level identification within 2 to 24hrs after blood culture bottle flagged positive.
Objectives:
To evaluate the turnaround time and accuracy for MALDI-TOF MS for identification of BSI.
To analyse the role of MALDI –TOF MS in antimicrobial stewardship focussing on early intervention and reduction in broad spectrum antibiotic use.
Material & Methodology
A retrospective observational study, which included all the blood culture sets received in the Department of Microbiology from February to July 2025. Samples were incubated in an automated BacT/ALERT 3D system (Biomerieux, France) and analysed after the system flagged them positive. Samples were analysed by Gram’s staining followed by inoculation in Blood agar, Chocolate agar and MacConkey agar as per standard protocols and kept for 18-24hrs incubation at 370C and chocodip as need be. Colonies were mounted on a slide and prepared for analysis using VITEK MS system software version 3.0 according to manufacturer’s instructions. The identification was considered correct if the confidence values were between 60% and 99.9%, as indicated by the manufacturer.
Result
Out of 3731 blood culture samples received, 402 cultures (10.77%) yielded growth while 1.1% (43 samples) were identified as contaminants, rate within acceptable quality standards (<3%) as per ASM guidelines. The contaminants were followed up with appropriate corrective and preventive action and taken as a routine AMS indicator for continuous follow up. Among the 402 positive cultures, 296 (73.6%) were Monobacterial, 38 (9.4%) had yeast growth and 68 samples (16.9%) were Polymicrobial. Among 296 Monobacterial isolates, 260 (87.8%) showed rapid identification by MALDI- TOF MS and 36 (12.1%) showed no result. Among 296 isolates, 31 blood culture sets were requested for Biofire Filmarray Blood culture identification panel (BCID II) and all the results (100%) correlated well with MALDI TOF. Genus level concordance was observed in 100% of samples (260/260) while species level concordance was 97.6% (254/260). The average turnaround reporting time from blood culture positivity to identification was 2- 24hrs. Antibiotic modifications were made in 32% (94) of patients after identification by MALDI- TOF MS. Appropriate targeted therapy was newly initiated in 19.5% (57) of patients. Descalation of antibiotics were happened in 12.5% (37) of patients. Cost of bacterial identification by MALDI-TOF MS was only 17-32% of the cost of conventional identification methods.
Conclusions
The integration of MALDI –TOF MS into BSI diagnostics significantly enhanced antimicrobial stewardship outcomes in our setting. By providing accurate species level identification within 2- 24hrs after culture positivity, MALDI -TOF MS enabled early identification,timely antibiotic optimization and cost effective stewardship impact.
Keywords: Antimicrobial stewardship, MALDI –TOF MS
Abstract 039 ASPICON 2025 |September 04 -07 | 2025 |
Faecal Microbiota Transplantation in the Management of MDR Gram-Negative Colonization: A Systematic Review
Yukesh R*, Sushil Sharma, Madhavrao C, Gaurav Manikrao Rangari, Arup Kumar Misra, Srinivasa Rao Katiboina
Department of Pharmacology, AIIMS Mangalagiri, Andhra Pradesh, India.
* Presenting author: yukeshrj@gmail.com
Background
The rise of multidrug-resistant (MDR) Gram-negative organisms like Carbapenem-Resistant Enterobacteriaceae (CRE), Extended-Spectrum Beta-Lactamase (ESBL) producers, and MDR Pseudomonas and Acinetobacter is a serious global health concern. These pathogens colonize the gut, serving as reservoirs for future infections, especially in immunocompromised patients. Antibiotics have limited success in decolonization and may harm the microbiome. Faecal microbiota transplantation (FMT) offers a promising, non-antibiotic strategy by restoring microbial diversity and colonization resistance.
Aims & Objectives: This systematic review aims to evaluate the clinical efficacy and safety of FMT in eradicating intestinal colonization with MDR Gram-negative organisms in human subjects.
Material & Methodology
We systematically searched PubMed, Scopus and Embase for studies published between January 2010 and July 2025. Search terms included combinations of “fecal microbiota transplantation” OR “FMT” AND “multidrug-resistant” AND (“Gram-negative” OR “Enterobacteriaceae” OR “CRE” OR “ESBL”). Eligible studies were clinical reports involving human subjects receiving FMT for decolonization of MDR Gram-negative organisms. Reviews, animal or in-vitro studies and those limited to Clostridium difficile infection (CDI) were excluded.
Result
A total of 28 studies (2 RCTs, 6 prospective, 3 retrospective, 2 case series, 15 case reports) involving around 360 patients aged 6 months to >70 years were included. Most were immunocompromised (Hematopoietic Stem Cell Transplantation, CDI, Spinal cord injury). Targeted organisms were mainly CRE/Carbapenemase-Producing Enterobacteriaceae and ESBL-E, with some Pseudomonas and Acinetobacter; Vancomycin-Resistant Enterococci frequently co-occurred. FMT protocols varied. Decolonization rates were 41% in RCTs (vs 29% controls), 37.5–87.5% in cohorts, 40–71% in case series, and often 100% in case reports. Adverse events were mostly mild, with one graft-versus-host disease. Meta-analysis was not feasible due to heterogeneity.
Conclusions
FMT shows considerable promise as a safe and effective strategy for gut decolonization of MDR Gram-negative organisms. Further large-scale trials and standardized protocols are needed to confirm its role in routine clinical practice
Abstract 040 ASPICON 2025 |September 04 -07 | 2025 |
Efficiency of Advanced Oxidation Processes (AOPs) in Removing Antibiotic Residues and Resistance Genes from Wastewater: A Systematic Review for Antimicrobial Stewardship Integration
Robin Reji*, Sushil Sharma, Madhavrao C, Arup Kumar Misra, Gaurav M Rangari, Srinivasa Rao K
Department of Pharmacology, AIIMS Mangalagiri, Andhra Pradesh, India.
* Presenting author: rrrobinhood55@gmail.com
Background
Antimicrobial resistance (AMR) poses a growing global health threat, undermining decades of progress in infectious disease control. While Antimicrobial Stewardship (AMS) programs have improved the rational use of antibiotics in clinical settings, environmental sources—particularly wastewater—serve as significant reservoirs of antibiotic residues and resistance genes (ARGs). Antibiotics, often excreted unmetabolized, enter municipal and hospital wastewater, where conventional treatment plants are inadequate for their complete removal. This allows sub-therapeutic antibiotic levels and ARGs to persist and promote resistance.
While AMS traditionally focusses on the judicial use of antimicrobials within the clinical setup, its scope must now include downstream interventions that can minimize the release and spread of potential determinants of resistance. Therefore, this systematic review aims to provide an insight into the removal efficiency of antibiotics residues and ARGs.
Aims & Objectives:
• To assess the removal efficiency (%) of antibiotic residues and the reduction of antibiotic‑resistance genes using different Advanced Oxidative Processes (AOPs)
• To identify any toxic transformation products formed during AOP treatment and their potential ecological risks and incorporate the findings into AMS framework
• To synthesize findings into recommendations, for integrating AOPs into a broader framework of AMS.
Material & Methodology
A systematic literature search (PubMed, Embase, Scopus) using a custom-made search string containing the keywords ‘Wastewater’, ‘Antibiotic Residue’, ‘Antibiotic Resistance Gene’ and ‘Advanced Oxidative Process’ identified 117 articles published from January 2020 to June 2025. 28 studies meeting inclusion criteria were reviewed.
Result
AOPs effectively reduce antibiotic residues, yet complete ARG removal is inconsistent. Moreover, high removal rates do not guarantee ecological safety, as residual antibiotic levels and increased effluent toxicity remain concerns. This highlights a disconnect between chemical degradation and biological risk mitigation.
Conclusions
AOPs hold promise for mitigating AMR through wastewater treatment. However, their application must extend beyond antibiotic degradation to address ARG persistence and ecotoxicity. A holistic, environmentally integrated AMS approach is vital.
Keywords: Antimicrobial Resistance; Advanced Oxidation Processes; Wastewater, Antibiotic Residues; Resistance Genes; Antimicrobial Stewardship; Ecopharmacology
Abstract 041 ASPICON 2025 |September 04 -07 | 2025 |
An Open-label, Randomized, Pragmatic Clinical Trial Comparing the Current Clinical Practices to Pharmacologist Guided Optimization of Antimicrobial Therapy Based on Average Creatinine-Urea Clearance in Critically-ill Patients- Interim analysis of a Pilot Study
Sanjeev Khanth P. E, Nitin R Gaikwad*, Chinmaya Panda, Yogendra Keche, Alok Singh, Pugazhenthan T, Vinay Rathore, Suprava Patel
All India Institute of Medical Sciences, Raipur, Chhattisgarh, India.
* Presenting author: nitingaikwad2707@aiimsraipur.edu.in
Background
Conventional dosing of renally cleared antimicrobials in critically-ill patients is complicated by fluctuating renal function, often resulting in sub-therapeutic exposure or toxicity. This may contribute to treatment failures, longer ICU stays, and antimicrobial resistance. Employing average creatinine-urea clearance (Avg. Cr-Ur Cl) to personalize dosing is a novel strategy, with limited clinical evidence to date.
Aims & Objectives: To rationalize the overuse/misuse of the reserve drugs in intensive care units and to avoid emergence of drug resistance.
Material & Methodology
This open-label, stratified-block randomized (1:1), pilot study was conducted in a tertiary care ICU (Oct 2024–June 2025). Adults (18–75 years) on ≥1 renally-cleared antimicrobial and likely to stay in CCU for >24h were randomized to intervention (pharmacologist-guided optimization using Avg. Cr-Ur Cl from 8-hour urine collection) or control (usual care). The primary outcome was change in SOFA score (ΔSOFA) at 72h and day 7. Key secondary outcomes includes, dose optimization events, ICU length-of-stay (LOS), 28-day mortality, ventilator-free days, antimicrobial consumption (DOT/LOT ratio).
Result
Thirty-two patients (SOFA < 10 vs ≥ 10) were randomized (Group A/intervention n=17, Group B/control n=15). At 72h, median ΔSOFA in SOFA ≥ 10 subgroup was –3 (–3, 0.5) in Group A vs –1 (–2.75, 1.5) in Group B; by day 7, –1 (–5.5, 3) vs –2.5 (–3.75, –1.25), respectively. Twenty dose optimization events occurred in Group A. Median ICU LOS was 7 (4.75, 8.75) days in Group A vs 10 (8, 26) in Group B in SOFA <10 subgroup; 28-day mortality was 40% vs 33.3%. Acceptance rate of recommendation was 83.3%.
Conclusions
Pharmacologist-guided dosing using Avg. Cr-Ur Cl is feasible with high acceptance (83.3%), reduces ΔSOFA at day 3 (SOFA ≥ 10) and shortens ICU stay, Challenges include multifactorial disease progression. Larger, adequately powered trials are warranted to confirm mortality and stewardship benefits.
Abstract 042 ASPICON 2025 |September 04 -07 | 2025 |
Adverse Drug Reactions to Vancomycin in the Paediatric Population: A Case Series
K N Abhinav Kaushal*, Bhuvana K, Sudha Reddy VR, Sarala N
Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, 563101, India
* Presenting author: kaushal.abhinav01@gmail.com
Background
Vancomycin is used in the management of gram-positive infections caused by Methicillin-Resistant Staphylococcus aureus (MRSA) and Clostridioides difficile. Despite its therapeutic benefits, vancomycin causes adverse drug reactions (ADRs), particularly hypersensitivity reactions such as Vancomycin Infusion Reaction (VIR) or “Red Man Syndrome.” VIR is a non-IgE-mediated pseudo-allergic reaction primarily linked to rapid infusion rates and mediated through Mas-related G protein-coupled receptor member X2 (MRGPRX2). Identifying such reactions in children, especially neonates, can be challenging due to nonspecific clinical features and underdeveloped immune responses. This case series highlights vancomycin-induced hypersensitivity reactions following intradermal test dose in infants and neonates which is an underreported occurrence, aiming to highlight early recognition, management, and implications for clinical practice.
Case Series
Fourteen paediatric patients aged between 22 days, and 18 months had hypersensitivity reactions following vancomycin administration, out of which 13 experienced it to test dose and one to first full dose. Symptoms resolved either spontaneously or after administration of pheniramine maleate in all cases. Based on clinical picture and culture sensitivity, vancomycin was discontinued in all children and alternate antimicrobials were administered.
Discussion
This case series highlights that adverse drug reactions (ADRs) in paediatric age group to vancomycin test dose, primarily presenting as rash, redness, and swelling. Despite changing brands after initial reactions, ADRs persisted in children. Both these brands were used in adults during this period, but no ADRs were reported. This difference may be due to MRGPRX2-mediated mast cell activation, with paediatric skin showing greater mast cell density, vascular permeability, and immature immune regulation, leading to local reactions.
Conclusion
Vancomycin-induced hypersensitivity in children, though usually mild, requires early recognition and proper management to avoid serious outcomes. Inspite of importance of test dose it is neglected at times which may result in unwanted consequences.
Abstract 043 ASPICON 2025 |September 04 -07 | 2025 |
Assessing the In–Vitro activity of Cefepime–Enmetazobactam and Plazomicin in ESBL and AmpC Beta Lactamase Co-Producing Enterobacterales Isolates Causing UTIs in a Tertiary Health-care Setup
Rajashree Choudhury*, Sumit Rai, Debabrata D, Priyadharshanni A
Department of Clinical Microbiology, AIIMS Mangalagiri, Mangalagiri, Guntur, Andhra Pradesh-522503, India.
* Presenting author: rajashreepito1996@gmail.com
Background
Enterobacterales producing ESBLs and ACBLs are resistant to oxyimino-cephalosporins and commonly cause urinary and bloodstream infections, complicating treatment. Their resistance genes, often present on plasmids, enable β-lactam antibiotic breakdown and are often linked to increased virulence and hence morbidity and mortality. Non-ACBL inducing carbapenems like Meropenem are often considered drugs of choice in upper UTI’s.
Cefepime, a fourth-generation cephalosporin, is approved for treating serious infections such as uUTI, cUTI, pyelonephritis, and pneumonia, especially caused by ACBLs; however, it is ineffective against ESBL-producing strains.
Enmetazobactam is a new penicillanic acid sulfone β-lactamase inhibitor (BLI), structurally similar to tazobactam, but with an added methyl group that gives it a zwitterionic (net neutral) charge, improving its ability to penetrate bacterial cells. It has a strong inhibitory activity against CTX-M, ESBLs, and other class A β-lactamases. Since cefepime is not significantly hydrolyzed by most AmpC and OXA β-lactamases, it serves as an ideal partner for combination with enmetazobactam, especially when they both have matching pharmacokinetics.
Plazomicin is a next-generation aminoglycoside antibiotic that targets the bacterial 30S ribosomal subunit, thus inhibiting protein synthesis with concentration-dependent kinetics. It has demonstrated potent efficacy against Enterobacterales, even those resistant to other aminoglycosides.
Aims & Objectives : Assessment of the in-vitro activity of Cefepime – Enmetazobactam and Plazomicin in ESBL and AmpC Beta Lactamase Co-Producing Enterobacterales causing UTI and their comparison with existing treatment options
Material & Methodology
Over a period of two months from May-June, 2025, urine samples from patients diagnosed with UTI were prospectively collected at a tertiary care hospital. Enterobacterales isolates were screened and confirmed for ESBL and AmpC coproduction using standard phenotypic methods. The in-vitro susceptibility to Cefepime-Enmetazobactam and Plazomicin was assessed using Kirby-Bauer disk diffusion (KBDD) method and interpreted using CLSI guidelines M100 35Ed.
Results
A total of 100 Enterobacterales ESBL + ACBL co-producing isolates were analysed in the study. Neither agents were found to be non-inferior in their in vitro efficacy against ESBL + ACBL co-producing isolates, and their efficacy was comparable to carbapenems.
Conclusion
This prospective observational study highlights the potent in vitro activity of Cefepime-Enmetazbactam and Plazomicin against ESBL and AmpC coproducing Enterobacterales in UTIs. These findings support their potential utility as therapeutic options in cases of antimicrobial resistance, especially as carbapenem-sparing drugs.
Abstract 044 ASPICON 2025 |September 04 -07 | 2025 |
Antibiotic Resistance Patterns in Vancomycin-Resistant Enterococci: A Systematic Review and Meta-Analysis Including Real-World Data from a Cancer Hospital in India
Gaurav Salunke*, Sanjay Biswas, Pradnya Samant, Shamita Binod, Jyoti Sinol
Department of Microbiology, Tata Memorial Hospital, Dr. E. Borges Road, Parel, Mumbai – 400012, India.
* Presenting author: drgsalunke@yahoo.com
Background
Vancomycin-resistant Enterococci (VRE) have emerged as significant nosocomial pathogens, especially in immunocompromised populations such as cancer patients. With increasing reliance on alternative agents like Linezolid, Daptomycin, Teicoplanin, and Tigecycline, understanding global resistance trends is critical for informed clinical decision-making.
Aims & Objectives: To assess global resistance patterns of VRE to key antibiotics (Linezolid, Daptomycin, Teicoplanin, Tigecycline) through a systematic review and meta-analysis, and to integrate real-world susceptibility data from a tertiary care cancer hospital in India
Material & Methodology
A systematic review of 30 Pub Med indexed studies reporting antibiotic susceptibility in VRE (E. faecium and E. faecalis) was conducted. Data on resistance rates to Linezolid, Daptomycin, Teicoplanin, and Tigecycline were extracted. Meta-analysis was performed using random-effects models. Heterogeneity was assessed via the I² statistic. Additionally, a retrospective analysis of antimicrobial susceptibility testing (AST) results from VITEK 2 (May 2021 – April 2025) was included from an oncology-focused microbiology laboratory, using 1,834 single, non-duplicate VRE isolates.
Results
Pooled resistance among VRE isolates was estimated as follows: Linezolid 3.1% (95% CI: 1.9–4.5%), Daptomycin 1.2% (95% CI: 0.4–2.3%), Teicoplanin 9.6% (95% CI: 6.3–13.8%), and Tigecycline 2.9% (95% CI: 1.6–4.8%). Resistance rates were higher in E. faecium compared to E. faecalis. The in-house cancer dataset (n=1,834) reported Linezolid resistance at 2.5% and Teicoplanin resistance at 7.2%, closely aligning with global estimates.
Conclusion
This meta-analysis confirms that resistance to Linezolid and Tigecycline remains low in VRE globally, while Teicoplanin resistance is more variable. The inclusion of cancer patient–specific data strengthens the clinical relevance of these findings and highlights the importance of continuous local surveillance to guide antimicrobial stewardship in high-risk populations.
Abstract 045 ASPICON 2025 |September 04 -07 | 2025 |
Comparative Effectiveness of Conventional and 3D-Bioprinted Biofilm Models in Studying Resistant Microbial Strains: A Meta-Analytic Review of Predictive and Clinical Outcomes
Krithikaa Sekar*, Jayakumar Subramaniam
Department of Microbiology, Saveetha Medical College, Saveetha Institute of Medical and Technical Sciences (SIMATS), Thandalam, Chennai, Tamil Nadu-602105, India.
* Presenting author: krithikaasekar@yahoo.in
Background
Antimicrobial resistance causes 1.3 million direct and 5 million indirect deaths annually- surpassing TB, HIV and malaria with estimated 39 million deaths and 28 million people in poverty by 2050. Nosocomial infections affect over 25% in developing countries, with 60.6% of isolates resistant and 40000 annual deaths. Biofilms cause 80% of chronic infections, resisting antimicrobials 10-1000x more than planktonic forms, forming in device and non-device infections (cystic fibrosis, diabetic foot etc.,). Factors like hydrodynamics, quorum-sensing and shear stress worsen outcomes: longer stays, ICU admissions, recurrence and 30-day mortality. Flow-cell systems enable biofilm study, but are low-throughput with imaging and removal issues. 3D-bioprinting offers customizable, realistic models, supporting robust biofilm formation and better in vivo simulation
Aims & Objectives:
1. Assess the predictive accuracy of conventional vs 3D-bioprinted flow-cell in stimulating in-vivo biofilm behavior
2. Assess methodological factors influencing model performance
3. Quantify key effect sizes to guide model selection for predicting treatment outcomes
Material & Methodology
We conducted PRISMA-guided systematic review (2008-2025) across PubMed, Scopus, and Web of Science comparing conventional and 3D-bioprinted flow-cell biofilm models of Pseudomonas aeruginosa, Escherichia coli, Staphylococcus aureus and Candida albicans. We used a random-effects model to calculate effect size and heterogeneity (I2).
Results
A total of 42 studies satisfied the inclusion criteria, showing enhanced growth (31.6-38.2%), biomass (18.6-25.6%), surface roughness (33.8-42.1%) and increased minimum biofilm inhibitory(4-8X) and eradication concentration(2-4X) indicating stronger biofilm resilience, lower treatment efficacy and infection persistence by 3D-bioprinting. There was a moderate heterogeneity (I2) (56%) due to differences in materials and microbial strains
Conclusion
3D-bioprinting enables accurate modelling of biofilm behavior, host-pathogen interactions, supports personalized therapies, antimicrobial stewardship (pre-treatment testing) and novel strategies (eg; nano-particles, photodynamic therapy, visco-elastic matrix targeting agents, CRISPR-Cas, quorum sensing inhibitors) to combat AMR.
Abstract 046 ASPICON 2025 |September 04 -07 | 2025 |
Evaluating the association between antibiotic consumption using Defined Daily Dose (DDD) score and Antibiogram to assess the prevalence of Antimicrobial Resistance (AMR) in a Tertiary Care Hospital: A Prospective, Observational Study
Vemparala Neha Chowdary*, Arup Kumar Misra
Department of Pharmacology, All India institute of Medical Sciences, Mangalagiri, Guntur, Andhra Pradesh, India.
* Presenting author: nehavemparala@gmail.com
Background
Antimicrobial Resistance (AMR) is a growing global throat, projected to cause over 10 million deaths annually by 2050. Misuse of antibiotics increases resistance, treatment costs, and harms both patients and hospital ecosystems. Effective control includes Antimicrobial Stewardship Programme’s (AMSPs), Infection Control Teams, WHO’s ATC/DDD metrics, Antibiogram, and AWaRe Classification. These tools guide proper antibiotic use, improve outcomes, and responsible antibiotic prescribing.
Aims & Objectives:
1. To estimate the usage of antimicrobials from inpatient hospital prescription database.
2. To assess the rationality of Antimicrobial’s usage based on AWaRe Classification.
3. To evaluate the relationship between Daily Defined Dose (DDD) with Antimicrobial Resistance (AMR) using Antibiogram.
Material & Methodology
The study will assess inpatient antibiotic use in a tertiary care hospital using WHO’s 2024 ATC/DDD index and AWaRe classification. Data on patient demographics, antibiotic usage, and microbiological tests will be collected. Antibiograms will be analyzed to correlate antibiotic consumption with resistance patterns.
Results
A study of 613 patients from 2 months revealed that most of them were aged 19-60 years (66.39%) and majority are males (54.48%). The average hospital stay was over 10 days for 48.45% of patients.
Piperacillin/Tazobactam had the highest consumption of 8410.5 grams among all the antimicrobials in the study though used in only 100 patients. The most used antimicrobial among the patients was Cefuroxime (n=392) with a total consumption of 2983.53 grams followed by Metronidazole (n=170). Among the Daily Defined Dose (DDD) of the individual drugs, Cefuroxime had the highest DDD of 1543.92 followed by Metronidazole.
Most antibiotics were from the Watch group (58.95%), followed by Access (35.42%), Reserve (1.2%).
Conclusion
An Antimicrobial Stewardship Program (AMSP) promotes safe antibiotic use, reducing resistance also aids hospitals in rational prescribing, reserving high-end antibiotics, and selecting proper antimicrobials using AWaRe classification. Incorporating DDD scores and antibiograms enhances treatment and prevents AMR. This approach yields a win-win situation for multiple disciplines to combat AMR.
Abstract Author Index
The number(s) following each author’s name indicate the corresponding abstract number.
Aishwarya D.Warang, 38 | Padmaja Nama, 1 | |
Akhila Chagalamari, 44 | Parandhaman A, 43 | |
Anika Malviya, 13 | Pradeep, 5 | |
Anusha B, 16 | Priyadharshanni A, 36 | |
Bharath Kumar G, 37 | R Rama Soujanya, 27 | |
Boda Srikanth Nayak, 20 | Rajashree Choudhury, 52 | |
Chithra C Nath, 2 | Robin Reji, 49 | |
Darshan B, 4 | Sarikonda Sandhya Rani, 35 | |
Gaurav Salunke, 53 | Sathiyanarayanan S, 30 | |
Hari Haran .G, 29 | Shilpa P, 3 | |
Harsha Suresh Mathew, 24 | Sree Sudha T Y, 18-19 | |
Hemanth Kumar, 40 | Sriram Kannuri, 28 | |
Iswarya M, 46-47 | Subalakshmi R, 23 | |
Jovita Davis Chirame, 42 | T. Prathyusha, 31-32 | |
K N Abhinav Kaushal, 51 | Vemparala Neha Chowdary, 56 | |
K. Yamin, 12 | Vennela Jyothi, 39 | |
Kanika Charan, 10-11 | Vijayalakshmi Gujapaneni, 6 | |
Krithikaa Sekar, 55 | Vindhya M, 25 | |
Mahesh Kumar B, 45 | Virendra Kumar Jaiswar, 22 | |
Manasa Sireesha Devara, 41 | Yukesh R, 48 | |
Mudita Khattri, 26 | ||
Naveen Murali, 9 | ||
Navi Nallasamy, 7 | ||
Navita Naik, 17 | ||
Nikhil John, 14-15 | ||
Nitin R Gaikwad, 50 |
