SASPI Ltd.
Pathogen vs Non-pathogen from a Culture-positive Report: How to Distinguish and Who Will?
JASPI September 2024/ Volume 2/Issue 3
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Panda PK, Yadav B, Sahu SN, Singh V.Pathogen vs Non-pathogen from a Culture-positive Report: How to Distinguish and Who Will? JASPI. 2024;2(3):-10-14 DOI: 10.62541/jaspi048
KEYWORDS: Pathogen; Commensal; Colonizer; Contaminant; Culture
INTRODUCTION
Recognizing microorganisms isolated in culture is one of the most challenging issues microbiologists and physicians face in infectious diseases.1 The crucial inquiry is to determine whether the microorganism under investigation is a genuine pathogen necessitating prompt medical attention, a commensal organism coexisting peacefully with the host, a colonizer perhaps dormant, or an unintentional contaminant brought in during specimen collection.
A pathogen is an organism that satisfies Koch’s postulates and serve as the definitive causative agent of disease.2,3
A non-pathogen is an organism that does not cause the host disease, harm, or death.4 Therefore, its presence does not warrant treatment with an antimicrobial agent.
Commensal, in contrast to a pathogen, engages in a symbiotic relationship with the host that does not result in perceptible, ongoing, or persistent harm.5 They are part of the microbiome; however, if the microbiota of one body area gains access to other areas, they may initiate pathogenesis at the new site.
Colonization denotes a state where a microorganism is present within the host for a variable duration without causing localized damage. Colonizers are microorganisms that do not belong to the host’s normal flora but do not inflict local damage to the host.6 Some patient characteristics contributing to the transformation of these microorganisms into pathogens are age ≥ 60 years, diabetes mellitus, acquired immunodeficiency syndrome, malignancy, foreign body in the urinary tract, or loss of vesicoureteral reflux on voiding cystourethrogram. Specific organism risk factors are also present.7
Contaminants include the unintended or accidental introduction of saprophytic organisms into clinical specimens, including bacteria, fungi, viruses, prions, protozoa, or their toxins and by-products.8
Bacteria involved in infectious diseases exist on a continuum, ranging from normal flora to external flora as bystanders, and finally to true pathogens. However, when a clinician receives a culture growth report on a provided sample, there is no distinction between these classified organisms in most cases. In rare instances, microbiologists and clinicians talk with each other before or after providing the report and finalize the true meaning of this growth. Sometimes, reports mention that contaminants cannot be ruled out; clinical co-relation needs to be done. Hence, microbiological diagnosis by culture is paramount to the clinician but sometimes without any real clinical significance.
Sterile body samples or fluids are biological samples that do not typically contain microorganisms, while non-sterile fluids may contain microorganisms. Infections in sterile body sites can be life-threatening and may result in severe morbidity and mortality.9,10 Examples of sterile body fluids include blood, cerebrospinal fluid, pleural fluid, peritoneal fluid, synovial fluid, and pericardial fluid. Non-sterile samples include sputum, urine, vomitus, or saliva. Specimens collected after surgical procedures inserting shunts, stents, or catheters may be colonized with microorganisms. Sometimes clinicians make different treatment decisions after the culture report becomes available based on their own practice. Moreover, there are no specific guidelines to answer this dilemma other than a framework for the optimal use of Microbiology laboratories in diagnosing infectious diseases, such as ‘Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2024 Update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM)’.11 This guideline advocates collaboration between clinicians and microbiologists, ensuring that the appropriate test is ordered and interpreted correctly and that results are integrated into patient care for timely diagnosis and treatment.
HOW TO SOLVE THE DILEMMA?
A recent study conducted on non-sterile urine samples by Yadav et al. approached a stepwise model to answer this dilemma of pathogen vs non-pathogen.12 It revealed that out of 275 samples analyzed, 249 were classified as pathogenic (90.54%). Among these, pathogenic commensals were 61.81%, pathogenic colonizers 14.18%, and direct pathogens 14.54%. On the other hand, among non-pathogenic cases of 9.46%, non-pathogenic commensals were 6.9%, non-pathogenic colonizers of 1.81%, and 0.72% as contaminants. In another similar study, in the same institute with a stepwise model (Figure 1A-B) by Sahu et al. (unpublished), examining 44 sterile blood samples, 27 included pathogenic colonizers, seven included direct pathogens, and 10 included non-pathogenic contaminants. These studies may help to come out of these dilemmas.
To optimize urine culture use, it is important to order them only when clinically indicated, such as when patients exhibit symptoms of a urinary tract infection (UTI), like dysuria, frequency, or flank pain. Urine cultures are appropriate for high-risk groups, including immunosuppression, pregnancy, or before urological procedures. Reducing unnecessary cultures can be achieved by following clinical guidelines and using reflex culturing, where cultures are performed only if initial screening tests, such as dipstick results, are positive.
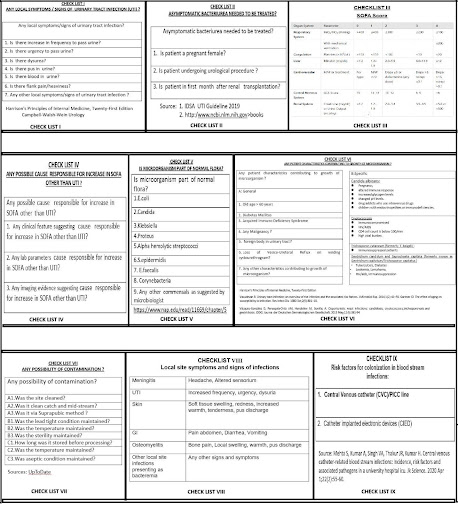
Figure 1: Stepwise model to decide pathogen vs non-pathogen in urine culture positive isolates (A) and blood culture positive isolates (B).

Urine microscopy, which detects pus cells (pyuria), can support diagnosis, but pyuria alone, without symptoms, should not trigger automatic culturing or treatment. In culture reporting, clinical microbiologists follow critical checks, including reviewing patient symptoms, assessing the time between sample collection and processing, evaluating the method of urine collection, analyzing colony counts to distinguish significant growth from contamination, and noting the presence of single or multiple morphotypes to determine actual infection. These steps ensure the accurate identification of relevant bacterial isolates for further testing. This approach improves diagnostic accuracy, reduces overtreatment, and helps combat antimicrobial resistance.
A critical component of this process is carefully considering the clinical presentation when ruling out infection. The clinician treats the patient based on their overall disease and symptoms, not merely relying on the laboratory report. The microbiologist’s role is to support the clinician in making a definitive diagnosis when infection is suspected and to guide appropriate therapy. By ensuring this close collaboration, diagnostic accuracy and patient care will improve while minimizing unnecessary antimicrobial use.11
Blood cultures and multiplex sepsis polymerase chain reaction are vital diagnostic tools in managing patients, especially for identifying underlying infectious processes. A significant challenge arises when blood cultures test positive, as it can be difficult to determine whether the isolated organism is a true pathogen or merely a contaminant or colonizer from a blood-bathed device. This dilemma mainly concerns increased healthcare costs and potential harm to patients.13 To address this issue, clinicians use a key approach: collecting blood samples in duplicate. This increases the test’s sensitivity and helps confirm the presence of a true pathogen.14 Additionally, microbiologists often advise a repeat blood sample to ensure that samples are collected under strict aseptic techniques when contamination is suspected.15 If the same organism is detected in the second sample, it is more likely to be a true pathogen rather than a contaminant. However, there is no definitive way to confirm colonization when a blood-bathed device is present and another source of infection exists, which often occurs in critically ill patients. However, clinician and microbiologist teams may use a bundle, checklist, or stepwise approach to solve this crucial dilemma (Figure 2), as evidenced by these recent studies.12
The patient’s clinical context plays a significant role in this decision-making process. Clinicians carefully evaluate the patient’s signs and symptoms, along with other laboratory findings such as complete blood count, procalcitonin, other infective biomarkers, erythrocyte sedimentation rate, and C-reactive protein levels, to determine whether the isolated organism is consistent with a true pathogen. Also, they use various sepsis scores to determine host-dysregulated responses such as Sequential Organ Failure Assessment (SOFA) score, Modified Early Warning Score (MEWS), etc.16 Certain organisms are generally considered contaminants, especially Gram-positive bacilli, common skin commensals. These bacteria can easily be introduced into culture plates during the laboratory processes. Additionally, if blood cultures become positive more than 72 hours after collection, the likelihood of contamination increases, depending on the organism. The use of antibiotics before obtaining blood cultures can also complicate the interpretation by delaying or preventing bacterial growth, making it essential to consider the presence of fastidious organisms like Kingella, Eikenella, Cardiobacterium, and species of Haemophilus, which require specific conditions for growth.16 Despite these challenges, some organisms are always regarded as true pathogens when isolated from blood cultures, such as Staphylococcus aureus, Group A streptococci, Streptococcus pneumoniae, Pseudomonas aeruginosa, Haemophilus influenzae, members of Enterobacteriaceae, Bacteroidaceae, and Candida species.17
Figure 2: Various checklists used in both stepwise models to decide pathogen vs non-pathogen in culture-positive samples (I-IX).
In the laboratory, samples are screened for quality. For example, those containing too many squamous epithelial cells in respiratory samples are often rejected due to possible contamination. Bartlett’s scoring, indicating more than 25 polymorphonuclear leukocytes and fewer than ten squamous epithelial cells per low-power field, strongly suggests the presence of a true pathogen.18 Similarly, in urine, the Kass Criteria are applied, which consider a bacterial count of ≥105 organisms per milliliter as indicative of significant bacteriuria.19 Pathogens isolated from fine needle aspirations and biopsies are always deemed significant. Pathogens like Aspergillus and Candida found in sputum are usually considered colonizers and are treated only if there is evidence of invasive disease. Any indwelling device in the respiratory or urinary tract always risks colonizer growth.8 For accurate diagnosis, semi-quantitative cultures are performed on lower respiratory tract or urine specimens. Depending on the specimen type and patient profile, growths with specific colony counts are considered significant.20 Urine is an excellent medium for bacterial growth, and any delay in processing can lead to bacterial proliferation, resulting in false-positive results.21 Hence, accurate diagnosis depends on proper specimen collection and prompt transportation and processing of samples to the laboratory, as evidenced in these recent studies.12
Although the above models look promising, there are a few limitations. The single-centre study had a small sample size and considered limited factors to decide the colonizer. Also, there were limitations of sepsis scores, an absolute method to determine contamination and a need to validate each step and its flow. Further, human assessment errors are a few apparent limitations.
CONCLUSIONS
Sterile and non-sterile body fluid infections are critical due to their life-threatening nature and high risk of morbidity and mortality. However, incorrect diagnoses can lead to unnecessary antimicrobial use, contributing to antimicrobial resistance (AMR), drug toxicity, and higher healthcare costs. Distinguishing between true pathogens and non-pathogens is of utmost importance. Clinician and microbiologist teams can collaboratively answer this complex decision-making process to categorize organisms and determine appropriate treatment strategies accurately. Adopting a structured stepwise model like the one mentioned above could be beneficial in addressing these challenges. Each hospital should consider implementing a flowchart tailored to its infection control program, antimicrobial stewardship practices, and local antibiograms. This model may include essential steps: Any local signs/symptoms suggestive of infection, any signs of septicaemia (by using SOFA/MEWS/any other score), any risk factors for the growth of the organism, what are commensals present in the sample site, any possibility of contaminants, and lastly response to empirical/culture guided treatment. This should remain adaptable, allowing for future modifications based on emerging evidence and evolving clinical needs. Establishing and refining such a model will improve patient outcomes and combat AMR.
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
REFERENCES
Lagier JC, Edouard S, Pagnier I, Mediannikov O, Drancourt M, Raoult D. Current and past strategies for bacterial culture in clinical microbiology. Clin Microbiol Rev. 2015;28(1):208-36.
Bhunjun CS, Phillips AJL, Jayawardena RS, Promputtha I, Hyde KD. Importance of Molecular Data to Identify Fungal Plant Pathogens and Guidelines for Pathogenicity Testing Based on Koch’s Postulates. Pathogens. 2021;10(9):1096.
Fredricks DN, Relman DA. Sequence-based identification of microbial pathogens: a reconsideration of Koch’s postulates. Clin Microbiol Rev. 1996;9(1):18-33.
Peterson JW. Bacterial Pathogenesis. In: Baron S, eds. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996.
Casadevall A, Pirofski LA. Host-pathogen interactions: basic concepts of microbial commensalism, colonization, infection, and disease. Infect Immun. 2000;68(12):6511-8.
von Graevenitz A. The role of opportunistic bacteria in human disease. Annu Rev Microbiol. 1977;31:447-71.
Vasudevan R. Urinary Tract Infection: An Overview of the Infection and the Associated Risk Factors. J Microbiol Exp. 2014;1:42–54.
Chatterjee A, Abraham J. Microbial contamination, prevention, and early detection in food industry. In: Holban AM, Grumezescu AM, eds. Microbial Contamination and Food Degradation. Academic Press; 2018:21-47.
Harshika Y K, Shobha M. K. R, Patil A B, Smita N R. A study on bacteriological profile and antimicrobial resistance pattern from various body fluids of patients attending the tertiary care Hospital, KIMS, Hubli. Indian J Microbiol Res. 2018;5(4):530-4.
Alfageme I, Muñoz F, Peña N, Umbría S. Empyema of the thorax in adults. Etiology, microbiologic findings, and management. Chest. 1993;103(3):839-43.
Miller JM, Binnicker MJ, Campbell S, et al. Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2024 Update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clin Infect Dis. Published online March 5, 2024.
Yadav B, Panda PK, Kant R, Omar BJ, Saini S, Panwar VK, Bahurupi YA. Understanding Clinical Variances in Urinary Isolates: Pathogenic vs. Non-Pathogenic Impacts in Tertiary Healthcare of North India. medRxiv. 2024:2024-01.
Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19(4):788-802.
Zhang C, Zheng X, Zhao C, et al. Detection of pathogenic microorganisms from bloodstream infection specimens using TaqMan array card technology. Sci Rep. 2018;8(1):12828.
Kristóf K, Pongrácz J. Interpretation of Blood Microbiology Results – Function of the Clinical Microbiologist. EJIFCC. 2016;27(2):147-55.
Nargis W, Ibrahim M, Ahamed BU. Procalcitonin versus C-reactive protein: Usefulness as biomarker of sepsis in ICU patient. Int J Crit Illn Inj Sci. 2014;4(3):195-9.
Chela HK, Vasudevan A, Rojas-Moreno C, Naqvi SH. Approach to Positive Blood Cultures in the Hospitalized Patient: A Review. Mo Med. 2019;116(4):313-7.
Murdoch DR, Morpeth SC, Hammitt LL, et al. Microscopic Analysis and Quality Assessment of Induced Sputum From Children With Pneumonia in the PERCH Study. Clin Infect Dis. 2017;64(suppl_3):S271-9.
Mandal J. Significance of Asymptomatic Bacteriuria. EMJ. 2017;2[3]:71-7.
Rattani S, Farooqi J, Jabeen G, et al. Evaluation of semi-quantitative compared to quantitative cultures of tracheal aspirates for the yield of culturable respiratory pathogens – a cross-sectional study. BMC Pulm Med. 2020;20(1):284.
Shokouhi S, Alavi Darazam I, Sadeghi M, Gachkar L, Dolatshahi S. Diagnostic Yield of a Direct Quantitative Smear of Lower Respiratory Tract Secretions in Patients with Suspected Pneumonia Compared to a Semi-quantitative Culture. Tanaffos. 2017;16(1):9-12.
Submit a Manuscript:
Copyright © Author(s) 2024. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

