WAAW 2023- The 6th Institutional Composite CMEs on Integrated Antimicrobial Stewardship Practices at AIIMS, Rishikesh
JASPI March 2024/ Volume 2/Issue 1
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Panda PK, Sharma M, Mishra R, et al.WAAW 2023- The 6th Institutional Composite CMEs on Integrated Antimicrobial Stewardship Practices at AIIMS, Rishikesh. JASPI. 2024;2(1):47-58 DOI: 10.62541/jaspi015
KEYWORDS: World antimicrobial awareness week, antimicrobial, resistance, stewardship, antibiogram
INTRODUCTION
The inappropriate use of antimicrobials is one of the world’s most pressing public health problems. Infectious organisms get adapted to the antimicrobials designed to kill them, making the drugs ineffective.1 People who get infected with organisms resistant to antimicrobials are more likely to have longer, more expensive hospital stays, and may be more likely to die as a result of an infection. It could cause 10 million deaths per year and an overall cost of $100 trillion to the global economy by 2050. The development of newer antibiotics is challenged at every step by the emerging antimicrobial resistance (AMR). The emergence of methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-intermediate Staphylococcus aureus (VISA), and superbugs like New Delhi metallo-beta- lactamase 1 positive Enterobacterales have compromised the most effective treatment leading to high mortality rate and fear of progression to the pre- antibiotic era.2 To curtail this major global health problem and to prevent further development of AMR a collaborative approach is required at different levels. Various measures for combating AMR can be directed at international, national, community, hospital, individual, and patient level. National Action Plan on AMR (NAP-AMR) 2017-2021 is an initiative from the Government of India to combat AMR.3 Strategic objectives of NAP-AMR are aligned with the global action plan on AMR (GAP-AMR) based on national needs and priorities.4 Among various options left to prevent AMR, ‘Integrated Antimicrobial Stewardship (IAS)’ is one of the cornerstones. Infection prevention stewardship, diagnostic stewardship, and antimicrobial stewardship, together constitute IAS, which is a coordinated program that promotes the right infection prevention and control practices, right diagnosis, and appropriate use of antimicrobials, improves patient outcomes, reduces microbial resistance, and decreases the spread of infections caused by Multidrug-resistant organisms.5 To give public awareness of AMR and do right practices, the World Health Organization (WHO) declared World Antibiotic Awareness Week (2015-2020); the name was changed to World Antimicrobial Awareness Week (2021-2022), this year to World AMR Awareness Week (WAAW), it is celebrated from 18- 24 November every year.
The aim of the celebration of World AMR Week at AIIMS, Rishikesh is to spread awareness regarding AMR and promote IAS practices among the general public and healthcare worker (HCW) and finally to draft a policy for better use of antimicrobials with the help of all departments (Department of Medicine, College of Nursing, Microbiology, Pharmacology, Community and Family Medicine and Nursing services) of the institute under the aegis of the Society of Antimicrobial Stewardship Practices in India (SASPI).
Table-1: Program Schedule of WAAW-2023
S.No. | Details | Day | Date | Venue | Beneficiaries |
| Saturday | 18.11.2023 | LT |
| |
| Sunday | 19.11.2023 |
| General Public & Pharmacist | |
| Monday | 20.11.2023 |
|
| |
for residents & faculty members | Tuesday | 21.11.2023 |
|
| |
for residents & faculty members | Wednesday | 22.11.2023 |
|
| |
| Thursday | 23.11.2023 | LT |
| |
| Friday | 24.11.2023 | LT | Pharmacy owners & CHO’s |
INAUGURATION AND WORKSHOP
On Day 1 (18th November 2023), World AMR Awareness Week was inaugurated by the Executive Director, Dean Academics, Medical Superintendent and other eminent dignitaries of AIIMS, Rishikesh which was followed by a workshop on IAS practices for HCW, in which more than 100 participants of clinicians, residents, nurses, and administrators have actively participated. The IAS foundation course was started for residents and faculty members in collaboration with SASPI (21-23 November, 3-hour sessions each day) and depicted in Table 1. The key sessions were as follows.
The core concept of integrated antimicrobial stewardship by Dr Prasan K Panda, Department of Medicine
Growing AMR associated with antimicrobial use is an increasing threat to healthcare and the global community. AMR requires a global solution. Therefore, improving awareness regarding AMR through effective communication, education and training, strengthening knowledge through surveillance and research, reducing the incidence of infection, optimizing the use of antimicrobial medicines in human and animal health and developing the economic case for sustainable investment (in AMR) were the few strategies discussed in this session to counter the AMR.
Clinician’s core competencies to become bedside steward by Dr Prativa Sahu and Dr Prasan K Panda, Department of Medicine
In clinical core competencies eight ‘Ds’ were discussed including the right diagnosis, drug, dose, delivery, decision on follow-up, monitoring patient response to treatment, ensuring infection control practices, right documentation and research. Also, various roles of HCWs towards the right eight ‘Ds’ of IAS practices were discussed in the presentation.
Clinical Antibiogram by Dr Vanya Singh, Department of Microbiology and Dr Sahil, Department of Medicine:
The need, types and components of clinical antibiograms were discussed. Also, why clinicians, microbiologists, and hospital administrators require the antibiogram was discussed in the deliberation. Table 2 represents the types of clinical antibiograms.
Table 2: Types of clinical antibiogram
Types | Definition | Data Presentation | Purpose | Clinical significance | Contextualization |
Cumulative | Represents overall antimicrobial susceptibility for all isolates combined within a specified location or timeframe | Presents combined susceptibility rates for all isolates without detailed subgroup breakdowns | Offers an overall view of antimicrobial resistance | Useful for general trends May miss clinically significant differences in specific patient groups or conditions. | Offers an overall summary of susceptibility patterns for all isolates combined |
Stratified | Segregates antimicrobial susceptibility data on specific parameters like patient demographics, specimen types. | Displays susceptibility data categorized by specific factors like patient age, specimen type, or clinical units, | Allows for the identification of subgroup-specific resistance trends | Provides nuanced data targeted antibiotic selection possible | Focuses on specific subgroup details, aiding in tailoring antibiotic therapy based on particular patient subsets or clinical scenarios |
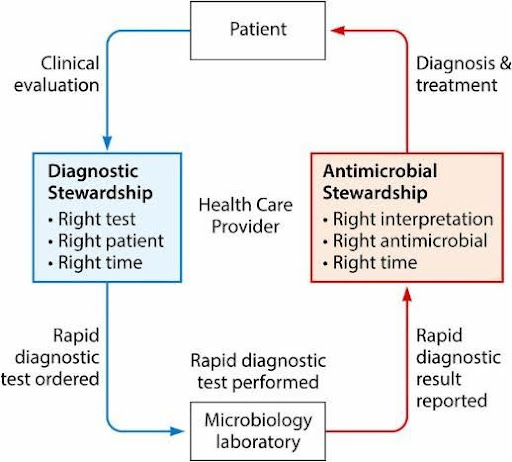
Diagnostic Stewardship by Dr. Vanya Singh and Dr Minakshi singh, Department of Microbiology
This deliberation highlighted the importance of right test by right method within the right time by emphasizing clinical and microbiology components. Pre-analytic, analytic and post analytic phases of diagnostic stewardship and methods of various sample collection, storage and transportation were discussed in details (Figure 1).
Figure 1: Diagnostic Stewardship process
Antimicrobial prophylaxis in surgery by Dr Amit K Tyagi, Department of ENT:
This session included discussions on antimicrobial surgical prophylaxis and appropriate antimicrobials to treat surgical site infections. Key highlights of the presentation on prerequisites and various categories of surgical antibiotics prophylaxis (SAP) are depicted in Figure 2 and Figure 3, respectively. The spectrum of coverage of prophylactic regimen for different wound categories is mentioned in Table 2
Figure 2: Key highlights of the presentation on prerequisites
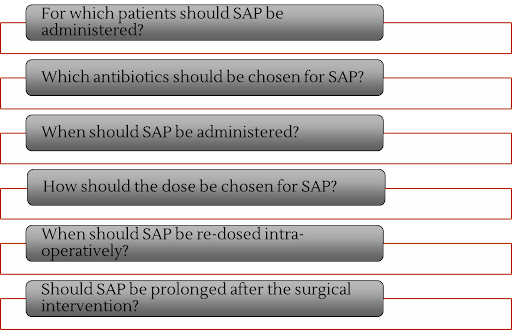
Figure 3: Various categories of surgical antibiotics prophylaxis (SAP)

Table 3: Category of wound and surgical prophylaxis
Surgical category | Likely pathogen | Spectrum of coverage |
Clean | Gram positive specially GPCs | Skin flora including staphylococci |
Clean contaminated | Gram Negative bacilli and enterococci | Enteric/ GU dictated by site |
Hospital Source Control: Unmet need of an Integrated Antimicrobial Stewardship Practice by Dr Rifika and Dr Prasan K Panda, Dept. of Medicine:
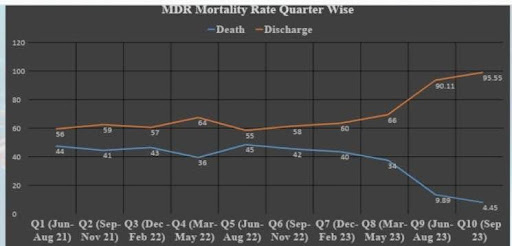
This session had a detailed discussion regarding the evolving significance of source control in healthcare, and the 5 ‘Ds’ of source control in healthcare care including drainage, debridement, device removal, definitive reconstruction and demarcation or isolation. Also, the source control as an integral component of IAS practices and steps to achieve the source control were the key highlights of the session. It was discussed how the institute has developed the PEAK-ME source control program and achieved >30% mortality reduction in 2 year time period (Figure 4). PEAK-ME includes common MDR organisms: Pseudomonas aeruginosa, Enterococcus faecium & faecalis, Acinetobacter baumannii, Klebsiella pneumoniae, MRSA (methicillin-resistant S. aureus), and Escherichia coli.
Figure 4: Reduction of mortality in MDR infections
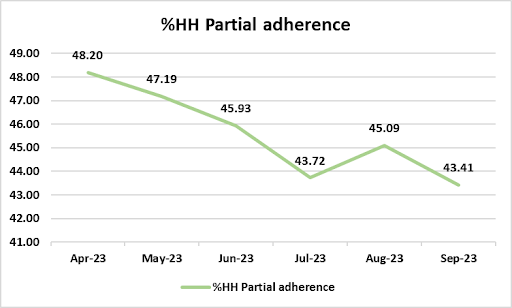
Health Care-Associated Infection (HAI) and Hand Hygiene by Dr Ambar Prasad, Dept of Microbiology and Infection Control Nurses, AIIMS, Rishikesh:
This session discussed health care-associated Infection (HAI), otherwise known as “nosocomial” or “hospital- acquired” infection. An infection occurs in a patient during the process of care in a hospital or other healthcare facility which was not present or incubating at the time of admission. This includes infections acquired in the health-care facility but appearing after discharge, and also occupational infection among health- care workers of the facility.
The most common site of infection and their risk factors and various preventive strategies including hand hygiene were the key point of discussion in the present session.
Hand hygiene compliance rates in the last six months are depicted in Figure 5.
Figure 5: Hand hygiene compliance rate
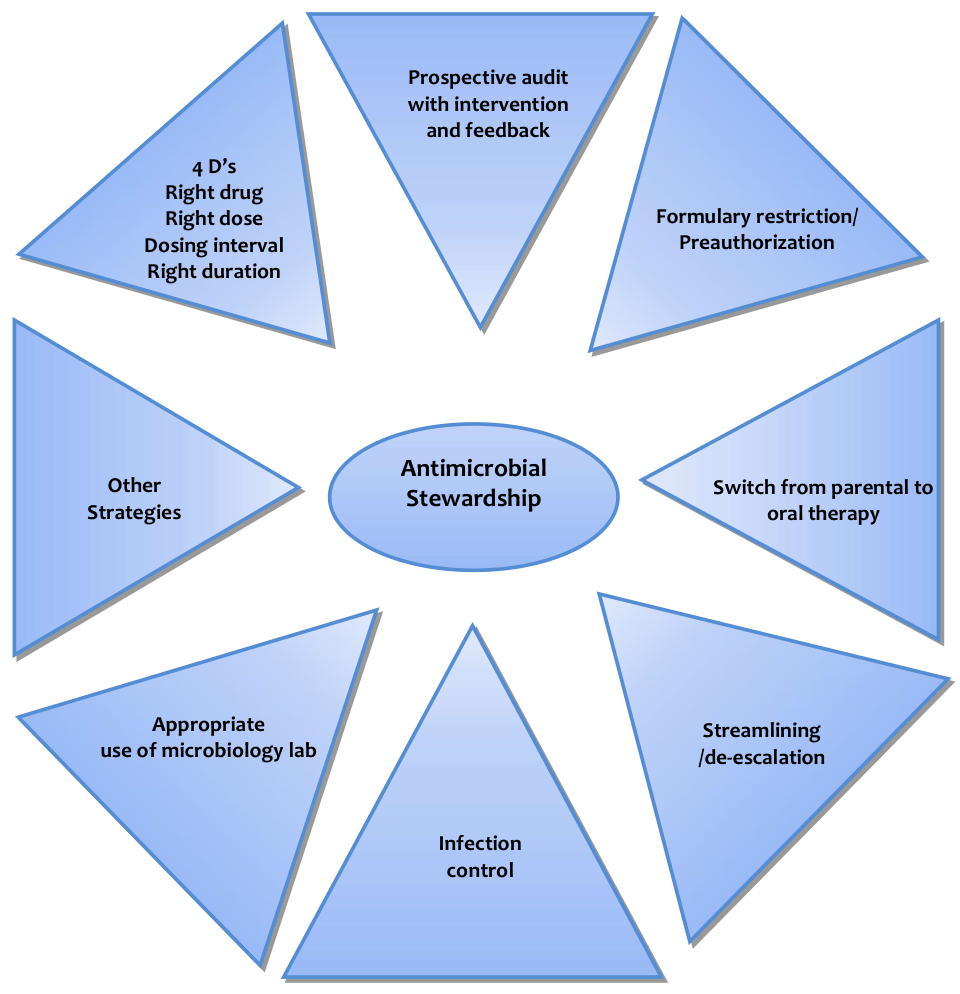
Prospective audit and feedback by Dr Puneet Dhamija, Dept of Pharmacology
In this session, two core strategies including front- end strategy and back-end strategy, pros and cons of preauthorization and prospective audit and feedback (Table 4) and components of the antimicrobial audit were discussed in detail (Figure 6).
Table 4: Types of stewardship audit
Pre-authorization | Prospective audit and feedback |
Advantages – Reduces empiric initiation of inappropriate Abx -Encourages early and frequent review of culture data -Reduces costs Disadvantages -May delay therapy -Loss of prescriber autonomy -Impacts only restricted agents | Advantages -More data is available and hence uptake is better -Educative and collaborative effort which could address de-escalation and duration of therapy -Prescriber autonomy is maintained Disadvantages –Labor intensive
-Compliance voluntary and prescriber reluctance to change if patient better |
Figure 6: Components of antimicrobial audit
IV to oral switch by Dr Puneet Dhamija, Dept of Pharmacology
For patients with a severe infection, it may be preferable to give intravenous (IV) antimicrobial treatment initially. If your patient is clinically improving and can adequately absorb oral medicines, they may be suitable to be switched early to oral administration known as I/V to oral switch. Recommendations for I/V to oral switch were discussed in detail (Table 5).
Why to switch??
Low risk of IV infusion-site infections (thrombophlebitis)
Lower cost of therapy
Decrease in the overall cost of treatment
Patient-friendly approach (early mobility, early discharge)
When to switch??
Antimicrobial treatment indicated
The patient has improved clinically
Oral intake (food and fluids) well-tolerated
Appropriate oral antibiotics are available
No indication for prolonged IV therapy or high tissue antibiotic concentration
Table 5: Recommendation for IV to oral switch
INTRAVENOUS | ORAL |
Benzylpenicillin 1.2g- 1.8g 6- hourly Amoxicillin 1-2g 8- hourly Ampicillin-sulbactam 1.5-3 g 6-hourly | Amoxicillin 1g 8-hourly Or AmoxIcillin-clavulanate 875/125mg 12-hourly |
AmoxIcillin-clavulanate 1.2g | AmoxIcillin-clavulanate 875/125mg 12-Hourly |
Cefuroxime 750mg-1.5g 8- hourly | Cefuroxime 500mg 12- hourly |
Ceftriaxone 1g – 2g daily | AmoxIcillin-clavulanate **875/125mg 12-hourly Or Cefuroxime 500mg 12- hourly (if respiratory infection) Or Cefixime 200mg 12-hourly or 400mg 24-hourly |
Cefazolin 1g-2g 8 hourly | Cefalexin 500mg-1g 6 hourly |
Piperacillin-tazobactam 4.5g 6 hourly OR 8 hourly | Amoxicillin-clavulanate 875/125mg 12-hourly 1 (Add ciprofloxacin 500- 750mg 12-hourly or levofloxacin 500-750 mg daily if specific Pseudomonas cover needed) |
Measurement of process and Outcome Indicators by Dr Bhupinder Solanki, Dept of Pharmacology
The components of AMS interventions are depicted in Figure 7.
The structural measure is to assess the capacity, systems and processes in a facility or an organization such as the establishment of leadership commitment, the record of AMS committee minutes, the number of meetings held, and reports issued to executives and other groups.
Process measure is to determine and quantify the day-to-day activities being conducted to drive improvement such as numbers of guidelines with dates of review or new point of care tools (e.g., clinical pathways) to implement and promote guideline concordant practice.
The outcome measure is to reduce the overall use of specific (broad-spectrum) antibiotics as well as no occurrence of unintended negative patient outcomes rather than improving the outcomes such as appropriateness of prescribing as per the guidelines.
Figure 7: Components of AMS intervention

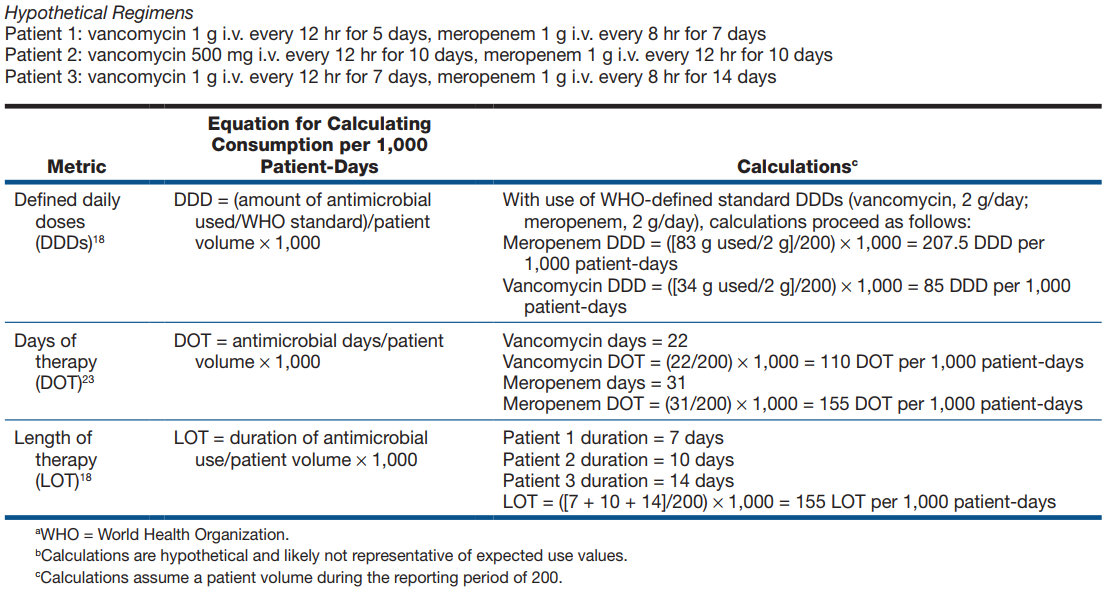
Metrics: Two main measures for amount are generally accepted, defined daily dose (DDD) and days of therapy (DOT). DDDs have been set by the WHO. DDD focuses on population-based parameters and assumes that patients and hospitals are homogenous entities.
Both methods (DDD & DOT) are standardized with a denominator such as hospitalized patient-days, and 1000 patient-days is the convention. While both strategies have limitations, the results frequently, though not always, correlate (Table 6).
Table 6: Various metrics used in AMS
Anti-microbial PK-PD in Clinical Practice by Dr Puneet Dhamija, Dept of Pharmacology
The basics of PK-PD in Clinical Practice are:
Minimum Inhibitory Concentration (MIC): Minimum concentration of the antibiotic drug able to inhibit the bacterial growth
Minimum Bactericidal Concentration (MBC): Minimum concentration of an antimicrobial agent that reduces the viability of the initial microorganism inoculation by ≥99.9%
Mutant Prevention Concentration (MPC): The threshold above which the selective proliferation of resistant mutants is expected to occur only rarely
The various PK-PD indices are mentioned in Figure 8.
Figure 8: PK-PD Indices

There is an urgent need for novel antibiotics to treat life-threatening infections caused by bacterial ‘superbugs’. Validated in vitro pharmacokinetic/pharmacodynamic (PK/PD) and animal infection models have been employed to identify the most predictive PK/PD indices and serve as key tools in the antibiotic development process (Figure 9).
Figure 9: Pharmacokinetic and Pharmacodynamic model

WALKATHON AND AWARENESS CAMPAIGN
On Day 2 (19th November 2023), a walkathon to spread awareness regarding AMR among the general public was organized, which was flagged off by Prof. Meenu Singh, Executive Director and around 200 HCWs participated. The route of the walkathon was from the Astha path to Awas Vikas colony and back to AIIMS, Rishikesh. Also on the same day, an awareness campaign was organized under the leadership of Dr Mahendra Singh, Dept of Community and Family Medicine along with the team.



ROLE PLAY ON ANTIMICROBIAL RESISTANCE, STEWARDSHIP AND VACCINATION
On Day 3 (20th November 2023), role play by nursing officers was organized to create awareness among the general public regarding antimicrobial resistance at OPD atrium, AIIMS, Rishikesh in the presence of Prof. R B Kalia, Medical Superintendent, Prof. Ravi Kant, Head of the Department of Medicine, Ms Reeta Sharma, Chief nursing officer, Dr Prasan K Panda and various other HCW’s. It was followed by panel discussion on preventing antimicrobial resistance together in the community area under the leadership of Dr Santosh Kumar, Additional Professor, Department of Community and Family Medicine.





 x
x
COMMUNITY AWARENESS CAMPAIGN AND ICE BREAKING SESSION WITH HCW’S
On Day 4 (21st November 2023), role play by nursing students under the leadership of Ms Rakhi Mishra, Assistant Professor, College of Nursing was organized to spread the message among patients and caregivers attending various OPDs. On the same day, ice breaking session was conducted by 33 teams comprising of faculty members/residents/infection control nurses/ other staff at various wards/units of AIIMS, Rishikesh to assess the AMR practice with the help of pre-validated checklist followed by 3 days’ foundation IAS course for faculty and residents.
On Day 5 (22nd November 2023), six teams comprising of professors, Deputy Nursing Superintendent and Assistant Nursing Superintendent visited the top 6 areas of IAS best practice to finalize the best IAS champion ward.
QUIZ AND POSTER COMPETITION FOR RESIDENTS, NURSES AND STUDENTS
On Day 6 (23rd of November 2023), a quiz and poster competition were organized for nurses, residents and students under the leadership of Dr Manisha Bist, Department of Pharmacology. Ms Niketa Kumari, Ms Alka Mittal and Ms Aarti Rana were the first, first and second runners respectively for the offline poster competition and Ms Deepika secured first position for the digital poster. Ms Sakshi and her team were the winners of the quiz competition. All the winners were awarded with certificates and mementoes the respective category
.





ROUND TABLE MEETING WITH PHARMACIST AND COMMUNITY HEALTH OFFICERS
On Day 7 (24th of November 2023), a round table meeting was held with local pharmacist and community health officers to facilitate righteous prescription and delivery of antimicrobials to combat with antimicrobial resistance, followed by valedictory session in which winners of various competitions and best IAS unit were awarded with mementos and certificates. Over all, in true sense team WAAW 2023 AIIMS, Rishikesh was able to comply and achieve the 2023 year theme “Preventing antimicrobial resistance together” by involving various departments under one umbrella of WAAW 2023.



CONCLUSION
A series of events were performed for entire WAAW 2023, which included workshop and foundation course on IAS practice and adult vaccination for health care workers, walkathon to spread public awareness about AMR, role play on vaccination and antimicrobial resistance, panel discussion in community area to create awareness among general public, ice breaking session and identification of IAS champion unit at AIIMS Rishikesh, poster, and quiz competition for residents, nurses and students, and round table meeting with local pharmacists and community health officers to create awareness on AMR. There were more than 1000 participants during this mega week of events. Further a remarkable collaboration was established by signing a Memorandum of Understanding (MoU) between SASPI and AIIMS Rishikesh to take the resolution of AMR and stewardship practices to next level where foundation IAS course was launched for residents and faculty members in presence of Prof. Meenu Singh, Executive director and CEO (AIIMS Rishikesh), Prof. Jaya Chaturvedi, Dean Academics (AIIMS, Rishikesh), Dr. Prasan K Panda, Secretory SASPI, Prof Shailendra Handu, Joint-Secretary SASPI, Prof Puneet Dhamija, Board of Directors SASPI, and other AIIMS and SASPI members. The participants took resolutions to continue IAS practices in their daily duties and to meet again to re- assess themselves during next WAAW (Figure 10).
Figure 10: AIIMS, Rishikesh resolutions by committed HCWs during WAAW 2023

ACKNOWLEDGEMENT
The AMR celebration from 18-24th of November 2023 was supported by Medical Superintendent (MS) office, and various departments of AIIMS, Rishikesh including Department of Medicine, Microbiology, Pharmacology, Community and Family Medicine, College of Nursing and CNO office. Team WAAW 23 would like to extend sincere gratitude to Prof. Meenu Singh, Executive Director and CEO and Prof Jaya Chaturvedi, Dean Academics AIIMS, Rishikesh for their guidance and endless support. Also, we would like to acknowledge the immense contribution and support of all the chairpersons Prof. Ravi Kant, Prof. Sailendra Handu, Prof. Smirti Arora, Prof. Vertika Saxena, Prof. Balram Omar and Ms. Reeta Sharma, organizing secretaries Dr Prasan K Panda, Mr. Maneesh Sharma, Dr Puneet Dhameja, Dr Ambar Prasad, Dr Santosh, Dr Mahendra and Dr Pooja Bhadoria, organizing joint-secretaries, Ms Rakhi Mishra, Dr Vanya singh, Ms. Kalpna and Ms. Vandana and other team members including Mr. Girirraj, Mr. Ashutosh, Ms. Deepa and Deputy Nursing Superintendents (DNS), Assistant Nursing Superintendents (ANS), Senior Nursing Officer (SNO), Nursing Officers (NO), Outreach cell, Media personnel, pharmacists, patients and their relatives and those who directly and indirectly were involved to make WAAW 23 a grand event.
CONFLICT OF INTERESTS STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
AUTHOR’S CONTRIBUTION
PKP: Methodology; Data curation; Analysis; Writing the draft
MS: Review & editing; Supervision; Validation
RM: Review & editing; Supervision; Validation
DK: Supervision; Review & editing
GS: Validation, Review & editing
AS: Validation, Review & editing
2. Kumar SG, Adithan C, Harish BN, Sujatha S, Roy G, Malini A. Antimicrobial resistance in India: A review. J Nat Sci Biol Med. 2013;4(2):286-91.
3. Ranjalkar J, Chandy SJ. India’s National Action Plan for antimicrobial resistance – An overview of the context, status, and way ahead. J Family Med Prim Care. 2019;8(6):1828
4. University of Washington. The burden of antimicrobial resistance (AMR) in India. Accessed December 25, 2023. https://www.healthdata.org/sites/default/files/f iles/Projects/GRAM/India_0.pdf
5. Chandy SJ, Michael JS, Veeraraghavan B, Abraham OC, Bachhav SS, Kshirsagar NA. ICMR programme on Antibiotic Stewardship, Prevention of Infection & Control (ASPIC). Indian J Med Res. 2014;139(2):226-30.
Submit a Manuscript:
Copyright © Author(s) 2024. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

