SASPI Ltd.
Prevalence of Device Associated Hospital Acquired Infection in a Medical Intensive Care Unit of a Tertiary Care Centre
JASPI December 2024/ Volume 2/Issue 4
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Bhushan D, Hegde AV, Kumar V, et al.Prevalence of Device Associated Hospital Acquired Infection in a Medical Intensive Care Unit of a Tertiary Care Centre. JASPI. 2024;2(4):46-52 DOI: 10.62541/jaspi056
ABSTRACT
Background: Infections acquired within a hospital setting, commonly called healthcare-associated infections (HAIs), are nosocomial infections that are typically absent or in an incubation phase upon admission. The study aimed to determine the prevalence of device-associated HAI and the factors affecting HAI in the Medical Intensive Care Unit (MICU).
Methods: A prospective observational study was conducted, including patients admitted to the MICU of a tertiary care medical centre from March 2020 to March 2023. The patient’s total ventilator days, catheter days, central line days, and development of HAI, according to the definition of surveillance, were recorded for each patient. Rates for device-associated infections and device utilisation ratios (DURs) were calculated. Statistical analysis involved descriptive statistics, Kaplan-Meier curve analysis with the Log Rank test, and logistic regression analysis to identify factors associated with HAI.
Results: 386 patients were included in the study, of which 52 (13.47%) developed HAI. The DUR for ventilators, catheters, and central lines were found to be 0.502, 0.949, and 0.545, respectively. Ventilator-associated pneumonia (VAP) rate was 16.07 per 1000 ventilator days, the catheter-associated urinary tract infection (CAUTI) rate was calculated to be 1.64 per 1000 catheter days, and the central line-associated bloodstream infection (CLABSI) rate was 1.91 per 1000 central line days. On multivariate analysis, the length of stay [adjusted odds ratio (AOR), 1.292; 95% CI: 1.200-1.391], and history of hospitalisation in the past 90 days (AOR, 6.556; 95% CI: 2.619-16.411) were also found to be independent predictors for HAI.
Conclusion: Our institution has lower rates of CAUTI and CLABSI. However, the VAP rate is higher than in studies conducted in an Indian setting. Hence, adopting the INICC multidimensional approach can address and reduce our VAP rate.
KEYWORDS: Intensive Care Units; Healthcare-associated infections; Pneumonia; Ventilator-associated; Catheter-related; CLABSI; Device-associated
Infections acquired within a hospital setting, commonly called healthcare-associated infections (HAIs), are nosocomial infections that are typically absent or in an incubation phase upon admission. These infections usually manifest post-hospitalisation, with symptoms emerging at least 48 hours after the patient’s admission to the healthcare facility.1
With the ever-increasing complexity of medical interventions, devices such as ventilators, catheters, and central lines have become integral to patient care. These life-saving devices risk acquired infection for the patient, significantly impacting in-hospital mortality.2 This usually results in a more extended hospital stay, leading to an even more significant economic burden on the patient. The incidence of HAI in an Indian study by Dasgupta et al. is around 13.6%. The prevalence varies in different studies as VAP accounts for 10.4 per 1000 ventilator days in Mehta et al., and CAUTI 9.4 per 1000 catheters per day in Pariher et al. It is estimated that HAIs cause a substantial economic burden per year, even in the United States, necessitating proper medical surveillance.3
Various measures have been employed to reduce the incidence of HAIs, including hand hygiene practices, maintaining a hygienic hospital environment, categorising patients based on risk factors, implementing robust public health surveillance systems, advocating for judicious antibiotic use, and ensuring adherence to established patient safety guidelines.4 Despite these various measures taken into account to reduce different types of HAIs, the prevalence of HAI in India remains higher. According to the International Nosocomial Infection Control Consortium (INICC), the prevalence of HAI in India is approximately 9.06 infections per 1,000 ICU patient days.5 Thus, understanding the dynamics of device-associated HAIs in ICUs is essential for implementing effective preventive measures and ensuring the safety of patients who rely on these critical medical interventions.
According to a literature review by Iyer et al. (2015), the prevalence of HAIs in India is impacted by challenges such as resource constraints, lack of standardised infection control practices, and the rising incidence of antimicrobial resistance.6
Therefore, this study is conducted to determine the prevalence of device-associated HAI and the factors affecting HAI in a tertiary care centre’s medical intensive care unit (ICU).
METHODOLOGY
Study design and setting
This prospective observational study was conducted in the medical intensive care unit (MICU) of the All India Institute of Medical Sciences, Patna, a tertiary care medical centre in eastern India, after approval from the Institute Ethics Committee (IEC).
Study participants
The study involved patients admitted to the MICU between March 2020 and March 2023.
Case definitions
CAUTI: Patients with any of the following with no alternative source: fever, rigors, new onset hypotension, confusion/ functional decline, and increased leucocytosis. New costovertebral tenderness/ pain, new supra pubic tenderness/ pain, pus around catheter insertion site AND any of the following – (A) If the catheter was removed in the past 2 days -clean catch urine culture with no more than two species of micro-organisms, at least one of which is bacteria of 100,000 or more colonies; in/out catheter urine culture with any number of micro-organisms, at least 1 of which is bacteria of 100 or more colonies (≥102 CFU/ml), (B) If an indwelling catheter is in place – then a positive urine culture with any number of microorganisms, at least 1 of which is bacteria of 100,000 colonies or more (105 CFU/ml).7
VAP: National Health Safety Network Pneumonia (NHSN PNU1) definition includes at least one of the following- new-onset fever (> 100.4 F), leucopenia/ leukocytosis, for adults> 70 years – altered mental status with no other cause. With at least one of the following in chest X-ray- new progressive infiltrates, consolidation, cavitation. And at least 2 of the following- new-onset purulent sputum, change in colour of sputum, increased suction requirement, increased respiratory secretion/ worsening gas exchange/ new onset or worsening cough/ dyspnea/ tachypnea, rails or bronchial breath sounds.7
CLABSI: patients with central venous catheter and Fever (> 100.4 F), chills, hypotension, and organisms identified in the blood are unrelated to an infection at another site. The same NHSN common commensal is determined by culture from two or more blood specimens collected separately.7
Inclusion criteria
1. Patients admitted to the MICU for any indication.
2. As per the definition of HAI, the minimum ICU stay is 48 hours.
3. Patients aged 15 years or older.
Exclusion criteria
1. Patients with evidence of any pre-existing HAI (i.e., HAI developed in the wards or at other hospitals).
Sampling technique
Complete enumeration: all patients admitted to the MICU during the study period meeting the inclusion criteria were included.
Study protocol
All patients admitted to the MICU were assessed for possible inclusion in the study. Informed consent was obtained from each participant or their first-degree relative if the patient was not mentally sound to provide consent. Surveillance was done during their stay in the ICU, and the following data was recorded:
1. Demographic parameters such as age and gender
2. Detailed history, including the presence of comorbidities and any history of hospitalisation in the past 90 days
3. Surveillance data includes ICU stay duration (patient days), ventilator days, catheter days, and central line days.
4. Clinical parameters, including intubation, the development of any HAI, and the outcome in terms of either a fatality or discharge from the MICU
Measures
The rates for device-associated infections were calculated. The VAP rate was calculated as the number of VAP cases per 1000 ventilator days.
The CAUTI rate was calculated as the number of CAUTI cases per 1000 catheter days.
The CLABSI rate was calculated as the number of CLABSI cases per 1000 central line days.
The device utilisation rates (DURs) for ventilators, catheters, and central lines were also calculated as the ratio of the number of days a device was used to the total patient days.
Statistical analysis
Data was entered in Microsoft Excel, cleaned, and coded. Analysis was performed using IBM SPSS ver. 26.0 (IBM Corp., Armonk, NY, USA). Categorical variables were expressed as frequencies and proportions. Kaplan-Meier curve analysis and Log Rank test were performed to calculate and compare the median survival times of patients who developed an HAI and those who did not.
A univariate binary logistic regression analysis was performed to look for factors associated with the development of HAI, and the variables with a p-value less than 0.2 were considered for the multivariate analysis model. The crude odds ratios with 95% confidence intervals (CI) were reported. The ‘Enter Method’ in SPSS was used to build the multivariate model, and the Hosmer-Lemeshow goodness of fit test assessed the model fit. The model variability was given by Nagelkerke’s R square (pseudo-R square). Adjusted odds ratios were calculated with their 95% CI. Statistical significance was attributed to p<0.05.
Ethics approval
This study was started after the approval of the Institute Ethics Committee with reference number AIIMS/Pat/IEC/PGTh/Jan21/21
RESULTS
A total of 386 patients were included in the study. Most of the patients, i.e., 166 (43.0%), belonged to the age group of 60–80 years, followed by 109 (28.2%) in the age category of 40–60 years. 218 (56.5%) were males. Most of the participants, i.e., 346 (89.9%), were admitted to the ICU for 2 weeks or less, and 300 (77.7 %) died during their stay. 52 (13.5%) individuals developed HAI (Table 1).
Table 1: Demographic details and clinical outcomes of the patients admitted to the ICU (N=386)
Variable | Categories | n (%) |
Age | Less than 20 | 12 (3.1) |
20 – 40 years | 73 (18.9) | |
40 – 60 years | 109 (28.2) | |
60 – 80 years | 166 (43.0) | |
80 -100 years | 26 (6.8) | |
Gender | Female | 168 (43.5) |
Male | 218 (56.5) | |
Length of ICU stay | 7 days or less | 207 (53.2) |
8 – 14 days | 142 (36.6) | |
15 – 28 days | 27 (7.8) | |
29 days or more | 9 (2.4) | |
Hospital-acquired infection | Yes | 52 (13.2) |
No | 334 (86.8) | |
Final Outcome | Death | 300 (77.7) |
Discharged (from ICU) | 86 (22.3) |
The total number of patient days (the sum of the total number of patients admitted to the ICU) was 3843 days. The DUR for ventilators, catheters, and central lines were found to be 0.502, 0.949, and 0.545, respectively. The VAP rate was 17.12 per 1000 ventilator days, the CAUTI rate was calculated to be 1.37 per 1000 catheter days, and the CLABSI rate was found to be 1.43 per 1000 central line days (Table 2).
Table 2: Summary of the surveillance data for ventilator-associated, catheter-associated, and central line-associated events.
Variable | Number of days (Total number of patient days = 3843) | Device utilization ratio | Number of events | Rate |
Ventilator days | 1929 | 0.502 | 33 | 17.12 per 1000 ventilator days |
Catheter days | 3646 | 0.949 | 5 | 1.37 per 1000 catheter days |
Central line days | 2094 | 0.545 | 3 | 1.43 per 1000 central line days |
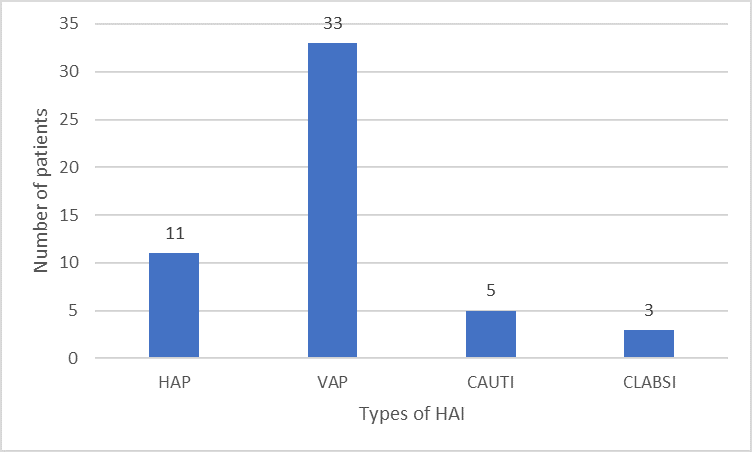
Among the 52 patients who developed HAI, 33 (63.5%) patients had VAP, 11 (21.2%) patients had HAP, 5(9.6%) patients had CAUTI, and 3 (5.7%) patients had CLABSI
(Figure 1).
Figure 1: The distribution of various types of hospital-acquired infections among the patients (n=52)
In our study, 261 out of 344 patients who didn’t have HAI succumbed, and 13 out of 52 who had HAI also succumbed. For total patients who expired, on Kaplan-Meier Curve analysis, it was seen that the median survival time in patients who did not develop HAI was 7 (95% CI: 6.518–7.582) days, while the median survival time in patients who did develop HAI was 17 (95% CI: 13.088–20.912) days (Figure 2).
Figure 2: Kaplan-Meier curves of patients in the ICU with and without hospital-acquired infection.
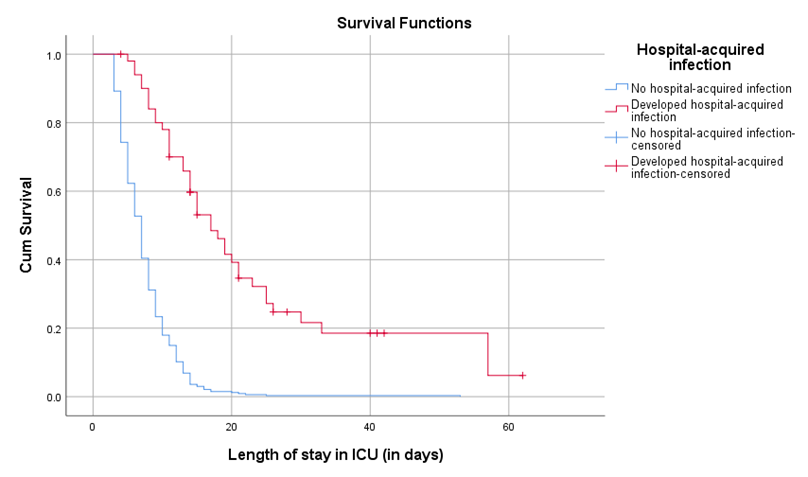
The Log Rank test revealed that there was a statistically significant difference between the curves [Chi-square=91.037 (at 1 degree of freedom) and p<0.001]. This paradox might suggest that those who stayed more in the ICU developed HAI, and those who did not develop HAI succumbed early due to their illness. More use of broad-spectrum higher antibiotics and other supportive measures in patients with HAI might have prolonged the stay but not overall survival.
On univariate logistic regression analysis, it was observed that the length of stay [crude odds ratio (COR), 1.254; 95% CI: 1.175-1.339], history of hospitalisation in the past 90 days (COR, 2.775; 95% CI: 1.442-5.337), and intubation (COR, 0.187; 95% CI: 0.101-0.346) were significant predictors of HAI.
On multivariate analysis, the length of stay [adjusted odds ratio (AOR), 1.292; 95% CI: 1.200–1.391], and history of hospitalisation in the past 90 days (AOR, 6.556; 95% CI: 2.619–16.411), were also found to be independent predictors for HAI (Table 3).
Table 3. Associates of hospital-acquired infection in ICU patients
Variable | Crude Odds | 95% Confidence Interval | p-value | Adjusted Odds | 95% Confidence Interval | p-value | ||
Lower Bound | Upper Bound | Lower Bound | Upper Bound | |||||
Age (in years) | 0.987 | 0.972 | 1.003 | 0.108 | 0.980 | 0.958 | 1.002 | 0.080 |
Female sex | 1.687 | 0.932 | 3.052 | 0.084 | 1.408 | 0.614 | 3.229 | 0.419 |
Length of stay (in days) | 1.254 | 1.175 | 1.339 | <0.001 | 1.292 | 1.200 | 1.391 | <0.001 |
History of hospitalization in the past 90 days | 2.775 | 1.442 | 5.337 | 0.002 | 6.556 | 2.619 | 16.411 | <0.001 |
Chi-square – 2.624 (df 8), p-value – 0.956
Nagelkerke R Square = 0.561
DISCUSSION
Our study screened 386 patients, and 52 patients developed HAI. VAP was the most prevalent HAI, followed by CAUTI and CLABSI (17.12 per 1000 ventilator days, 1.43 per 1000 central line days, and 1.37 per 1000 catheter days were the VAP, CLABSI, and CAUTI rates, respectively). Length of stay, history of hospitalisation in the past 90 days, and intubation were independent predictors of HAI.
HAIs pose a significant challenge in the management of ICU patients, thus requiring proper surveillance. The incidence of HAI in our study (13.2%) is comparable to a survey by Dasgupta S. et al. in the ICU setting in eastern India (11.98%).8 However, the incidences of CAUTI were lower compared to other Indian studies.9-11
The VAP rate found in our study (17.12 per 1000 ventilator days) is higher than the VAP rate evaluated in other Indian cities (10.4 per 1000 ventilator days),12-13 and other Southeast Asian countries.14-15 However, the VAP rate observed in our study is like the pooled mean VAP rate observed (16.3 per 1,000 device days) in 43 countries.16 This high rate of VAP can be due to a lack of Infection control practices in the ICU, cross-contamination and the non-availability of isolation facilities in the ICU. The INICC-developed multimodal approach for the prevention of VAP should be used. It has six main parts: (1) bundle care, which has 10 elements to prevent pneumonia; (2) educational programmes; (3) outcomes monitoring; (4) online process surveillance to see how healthy bundles are being followed; (5) giving feedback on VAP rates and their effects; and (6) performance feedback.17
The Device Utilisation Ratio (DUR) is a measure that assesses the usage of a medical device in a healthcare setting.18 DUR is a decisive factor known for its positive correlation with HAI. In 2014, the National Healthcare Safety Network (NHSN) reported a DUR of 0.44, less than the DUR of the endotracheal tube observed at our study site, which stands at 0.502. This can be attributed to the transfer of more complex cases from all over the state, as our centre is one of the three tertiary care centres in Bihar, the third most populated state of the nation.
More than five million patients globally in intensive care hospital environments experience the insertion of urinary catheters, elevating their susceptibility to CAUTI.19 The CAUTI rate in our study is 1.37 per 1000 catheter days, which is very low compared to the study done in an Indian setting by Parihar S. et al. (9.4 per 1000 urinary catheter days).20 A survey by Letica-Kriegel A. S. et al. reported a similar CAUTI rate compared to our institution.21 This can be attributed to adequately implementing hand hygiene, infection control, and catheter care bundles. The DUR for catheter utilisation in our study is 0.9, which is very high compared to the INICC report. This can be attributed to the severity of cases treated at tertiary-level referral hospitals requiring output monitoring.
The central line is one of the most common procedures done in the ICU setting, and CLABSIs are associated with significant morbidity and mortality in the patient, ultimately causing increased healthcare costs. The CLABSI rate in our study was 1.43 per 1000 central line days, which is lower than the rate reported by INICC (4.47 per 1000 central line days) and about the same as the rate reported by Rosenthal V. D. in the US (1.6 per 1000 central line days).22 Our study’s central line utilisation rate is 0.545, similar to the INICC report (0.53). CLABSI is the most preventable form of HAI infection, and its incidence is higher in developing countries. The low rate of CLABSI can be attributed to the incorporation of quality aseptic precaution methods, skilled healthcare workers, and compliance with the insertion bundle method in the hospital’s culture and policies.
Risk factors like length of hospital stay and history of hospitalisation in the past 90 days are the independent risk factors that cause an increase in the incidence of HAIs. HAI was found to be shared in advancing age and females, but they didn’t show statistical significance. Among device-associated HAIs, VAP is a major contributor to prolonged patient stays. Stewart S. et al. highlight that preventing a single HAI can result in an average reduction of 7.8 days in hospital stay. Consequently, preventing HAIs diminishes the length of stay. It contributes to the availability of hospital beds to treat additional patients—a particularly valuable outcome in countries with high patient loads, such as India.23-25
There are some limitations to this study as well. Since this study was conducted at a single centre, its findings may not be generalised to other institutions. Other limitations are the recruitment from the medical ICU, the inability to include pediatric patients, and the failure to assess the quality of infection control practice among healthcare workers. Certain suspected cases of bloodstream infections and CAUTI in whom initial cultures were sterile were missed because of their untimely death or due to leave against medical advice (LAMA). However, it’s worth noting that our study included a large sample size, which helps mitigate the potential for selection bias.
CONCLUSION
While our medicine ICU has lower rates of CAUTI and CLABSI, it is noteworthy that the VAP rate is higher compared to studies conducted in the Indian setting. Hence, adopting the INICC multidimensional approach can address and reduce our VAP rate. The device utilisation rate is also high at our centre, which needs to be dealt with through training and education of healthcare workers, audits and protocol-wise care in the Intensive care unit.
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
AUTHOR’S CONTRIBUTION
DV: Concept, methodology, write-up of article, analysis
AVH: Data collection and analysis, writing of project
VK: Conceptualisation, write-up review, discussion
BT: Methodology write-up, concept to detailed project preparation
PK: Methodology write-up, concept to detailed project preparation, analysis
SV: Data collection and write up
JA: Data collection and write up
REFERENCES
Monegro AF, Muppidi V, Regunath H. Hospital-Acquired Infections. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 12, 2023.
Blot S, Ruppé E, Harbarth S, et al. Healthcare-associated infections in adult intensive care unit patients: Changes in epidemiology, diagnosis, prevention and contributions of new technologies. Intensive Crit Care Nurs. 2022;70:103227.
Stone PW. Economic burden of healthcare-associated infections: an American perspective. Expert Rev Pharmacoecon Outcomes Res. 2009;9(5):417-22.
Patil SJ, Ambulkar R, Kulkarni AP. Patient Safety in Intensive Care Unit: What can We Do Better? Indian J Crit Care Med. 2023;27(3):163-5.
Haque M, McKimm J, Sartelli M, et al. Strategies to Prevent Healthcare-Associated Infections: A Narrative Overview. Risk Manag Healthc Policy. 2020;13:1765-80.
Iyer V, Sewlikar S, Desai A. Healthcare acquired infection in India – A literature review. J Microbiol Immunol Infect. 2015;48(2, Suppl 1):S182.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting [published correction appears in Am J Infect Control. 2008 Nov;36(9):655]. Am J Infect Control. 2008;36(5):309-32.
Dasgupta S, Das S, Chawan NS, Hazra A. Nosocomial infections in the intensive care unit: Incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med. 2015;19(1):14-20.
Parihar S, Sharma R, Kinimi SV, Choudhary S. An Observational Study from Northern India to Evaluate Catheter-associated Urinary Tract Infection in Medical Intensive Care Unit at a Tertiary Care Center. Indian J Crit Care Med. 2023;27(9):642-6.
Mehta Y, Jaggi N, Rosenthal VD, et al. Device-Associated Infection Rates in 20 Cities of India, Data Summary for 2004-2013: Findings of the International Nosocomial Infection Control Consortium. Infect Control Hosp Epidemiol. 2016;37(2):172-81.
Behera B, Jena J, Mahapatra A, Biswala J. Impact of modified CDC/NHSN surveillance definition on the incidence of CAUTI: a study from an Indian tertiary care hospital. J Infect Prev. 2021;22(4):162-5.
Mehta Y, Jaggi N, Rosenthal VD, et al. Device-Associated Infection Rates in 20 Cities of India, Data Summary for 2004-2013: Findings of the International Nosocomial Infection Control Consortium. Infect Control Hosp Epidemiol. 2016;37(2):172-81.
Mumtaz H, Saqib M, Khan W, et al. Ventilator-associated pneumonia in intensive care unit patients: a systematic review. Ann Med Surg (Lond). 2023;85(6):2932-9.
Kharel S, Bist A, Mishra SK. Ventilator-associated pneumonia among ICU patients in WHO Southeast Asian region: A systematic review. PLoS One. 2021;16(3):e0247832.
Gadani H, Vyas A, Kar AK. A study of ventilator-associated pneumonia: Incidence, outcome, risk factors and measures to be taken for prevention. Indian J Anaesth. 2010;54(6):535-40.
Rosenthal VD, Maki DG, Mehta Y, et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 43 countries for 2007-2012. Device-associated module [published correction appears in Am J Infect Control. 2015 Jul;43(7):779-81]. Am J Infect Control. 2014;42(9):942-56.
Rosenthal VD. International Nosocomial Infection Control Consortium (INICC) resources: INICC multidimensional approach and INICC surveillance online system. Am J Infect Control. 2016;44(6):e81-90.
Kim EJ, Kwak YG, Park SH, et al. Trends in device utilization ratios in intensive care units over 10-year period in South Korea: device utilization ratio as a new aspect of surveillance. J Hosp Infect. 2018;100(3):e169-77.
Danchaivijitr S, Dhiraputra C, Cherdrungsi R, Jintanothaitavorn D, Srihapol N. Catheter-associated urinary tract infection. J Med Assoc Thai. 2005;88 Suppl 10:S26-30.
Parihar S, Sharma R, Kinimi SV, Choudhary S. An Observational Study from Northern India to Evaluate Catheter-associated Urinary Tract Infection in Medical Intensive Care Unit at a Tertiary Care Center. Indian J Crit Care Med. 2023;27(9):642-6.
Letica-Kriegel AS, Salmasian H, Vawdrey DK, et al. Identifying the risk factors for catheter-associated urinary tract infections: a large cross-sectional study of six hospitals. BMJ Open. 2019;9(2):e022137.
Rosenthal VD. Central line-associated bloodstream infections in limited-resource countries: a review of the literature. Clin Infect Dis. 2009;49(12):1899-907.
Stewart S, Robertson C, Pan J, et al. Impact of healthcare-associated infection on length of stay. J Hosp Infect. 2021;114:23-31.
Jia H, Li L, Li W, et al. Impact of Healthcare-Associated Infections on Length of Stay: A Study in 68 Hospitals in China. Biomed Res Int. 2019;2019:2590563.
Graves N. Economics and preventing hospital-acquired infection. Emerg Infect Dis. 2004;10(4):561-6.
Submit a Manuscript:
Copyright © Author(s) 2024. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

