Peer Tutoring of Healthcare Staff to Improve Infection Prevention and Control Practices – A Quasi-Experimental Study in Low-Resource Teaching Hospitals
JASPI March 2025 / Volume 3 /Issue 1
Copyright: © Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Khan F, Arsalan, Ahmed S, Shah MS, Khan T.Peer Tutoring of Healthcare Staff to Improve Infection Prevention and Control Practices – A Quasi Experimental Study in Low-Resource Teaching Hospitals. JASPI. 2025;3(1):20-25 DOI: 10.62541/jaspi071
ABSTRACT
Background: Infection prevention and control practices are critical in healthcare to reduce healthcare-associated infections (HAIs). In low-resource settings, limited trained personnel impede effective implementation. This study assessed a peer tutoring program in which nursing staff trained their peers in infection prevention and control.
Method: This educational intervention, a quasi-experimental study, was conducted in a low-resource teaching hospital, involving nursing staff as both tutors and tutees. Tutors received preparation through a Faculty Development Program (FDP) and led infection prevention and control sessions. Evaluation tools included pre- and post-tests, tutor assessments, and satisfaction surveys from 134 participants.
Results: Post-test scores significantly increased from 56.05% to 73.4%, showing improved infection prevention and control knowledge. Tutees reported greater confidence, with 73% rating the program as “Excellent.” Tutors exhibited strong communication and mastery, though time management and teaching aid use required improvement.
Conclusion: Peer tutoring effectively enhances infection prevention and control knowledge and compliance in low-resource settings, fostering skill transfer and potentially reducing HAIs.
KEYWORDS: Peer Tutoring; Infection prevention and control; Healthcare staff
INTRODUCTION
Teaching and training of the healthcare staff for infection prevention and control practices is essential to increase their knowledge, competency, and practical skills about infectious diseases and their prevention.1 Understanding the rationale for Infection Prevention and Control (ICP) practices can increase Health Care Professionals’ (HCP) adherence to, and acceptance of those practices.2 However, in most government hospitals, there are no dedicated teaching staff for the same. Active members of the Hospital Infection Prevention and Control Committee overtake this task solely based on their motivation. The scarcity of teaching staff for training the healthcare professionals leads to reduced motivation among HCPs in following Infection prevention and control practices due to lack of training. The consequences of this can be higher chances of healthcare-associated infections, Longer duration of stay of patients, higher financial burden on the patient and on the hospital and increased antimicrobial resistance. Alternative solutions that do not draw on already limited faculty resources are required to ensure that the healthcare staffs obtain the skills and knowledge required to follow the standard infection prevention and control practices. Peer tutoring may be one method of addressing this issue. Peer tutoring or peer-assisted learning (PAL), after generating a great deal of scholarly interest, has now become a well-established educational modality.3 Peer tutoring in infection prevention and control practices can have short-term impacts like higher compliance to infection prevention and control practices by the trained healthcare professionals, which can further materialize into many long-term impacts like behavioural change among the healthcare professionals in institution(s) with scarce resources, better patient outcome due to reduced rate of healthcare-associated infections, decreased length of hospital stay and decreased financial burden on patient and healthcare system and decreased antimicrobial resistance. The present study was conducted with the following aims and objectives:
To assess the perception of the Faculty Development Program (FDP) conducted for motivated HCPs;
To assess tutees’ perceptions of a formal peer tutoring program;
To examine how nursing staff experienced and evaluated their roles as tutors;
To analyze learning of HCP participating in FDP by pre-test and post-test;
To analyze learning of tutees in peer tutoring program;
METHODOLOGY
Study Design: This prospective educational interventional study was a quasi-experimental study conducted over a six-month period at Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh. The study aimed to assess the effectiveness of a peer tutoring intervention for improving infection prevention and control practices among nursing staffs.
Participants: The study involved 134 nursing staff members (including faculty and nursing staff members in different departments). A simple random sampling technique was used to select participants from the nursing staff to ensure a representative sample. Participants were required to meet inclusion criteria (e.g., active employment, willingness to participate), and were randomly assigned to tutor or tutee roles.
Intervention: Several tools were employed for data collection to assess both the intervention’s effectiveness and the tutors’ performance. These included:
Pre- and post-test questionnaires: To evaluate the changes in knowledge of infection prevention and control practices before and after the intervention.
Satisfaction surveys: To assess the participants’ satisfaction with the peer tutoring sessions.
Checklist-based observations by members of the HICC and Medical Education Unit (MEU): To monitor the quality of tutoring sessions.
Video Assessment of Interactions and Learning (VAIL): To evaluate the interaction quality between tutors and tutees.
In-depth interviews: Conducted with tutors to assess their performance and the effectiveness of the training.
Comparator: The comparison of pre- and post-intervention knowledge levels served to evaluate the effectiveness of the peer tutoring model. Additionally, routine infection prevention and control training (limited and irregular due to faculty constraints) functioned as the baseline standard for comparison.
Outcomes:
Primary Outcome:
Improvement in knowledge of infection prevention and control (IPC) practices, measured by the difference between pre-test and post-test scores.
Secondary Outcomes:
Tutees’ satisfaction levels, assessed using a Likert scale.
Tutors’ performance evaluation, focusing on self-confidence, communication skills, subject command, time management, and use of teaching aids.
Perception of peer tutoring among healthcare staff, gathered through opinion polls.
Tutors’ self-assessment and feedback from the Hospital Infection Control Committee (HICC) and Medical Education Unit (MEU).
Engagement and confidence reported by participants post-intervention.
Ethical Considerations: Ethical approval for the study was obtained from the institutional ethics committee (Institutional Review Board, AMU), and informed consent was obtained from all participants. The study adhered to ethical guidelines, ensuring confidentiality and voluntary participation.
Diversity, Equity, and Inclusion: The study actively considered issues of diversity, equity, and inclusion. Participants from diverse backgrounds were included. The random sampling approach ensured diversity in the participant pool. The study’s design and analysis aimed to evaluate the intervention’s effectiveness across diverse groups, with particular attention to how the intervention may benefit participants from different demographic groups.
RESULTS
We included 134 healthcare staff members, primarily nursing faculty, as tutees in the peer tutoring program. Among them, 10 staff members demonstrated high competency in infection prevention and control practices (assessment score >75%) and were selected as tutors after completing the Faculty Development Program (FDP).
We evaluated tutors on several competencies essential for effective peer tutoring. The evaluation revealed strengths and areas for improvement:
Self-confidence: Tutors exhibited high self-confidence, which significantly enhanced their communication and engagement with peers, stemming from prior experience and familiarity with the subject matter.
Communication Skills: Strong communication skills ensured that information was clearly conveyed to tutees, reflected in high scores on the satisfaction questionnaire.
Real-Life Experience: Tutors effectively linked theoretical knowledge to practical examples, making sessions more relatable.
Areas for Improvement: Time management was the most significant area where they were lacking.
Time Management: Some tutors struggled to manage the allocated time, resulting in rushed sessions or incomplete content coverage.
Utilization of Teaching Aids: Despite having access to teaching aids like PowerPoint presentations, tutors struggled with optimal integration, which affected session delivery.
Trainees’ Satisfaction and Learning Outcomes: Tutees rated the sessions on a Likert scale, revealing significant insights:
Punctuality: Sessions generally started and ended on time, indicating effective time management, though variability was noted among tutors.
Subject Command: Tutees rated tutors highly in subject command, particularly in hand hygiene, biomedical waste management, and safe injection practices, demonstrating the effectiveness of the peer tutoring model.
Teaching Methods: While many tutees appreciated innovative teaching methods, feedback suggested that consistent use of such methods across all sessions would further enhance learning.
Overall Satisfaction: Most trainees (73%) rated the program as “Excellent,” with 19% and 7% rating it as “Very Good” and “Good,” respectively (Figure 1). This high satisfaction underscores the program’s positive impact on understanding infection prevention and control practices.
Figure 1: Scoring by the trainees on the Likert Scale.

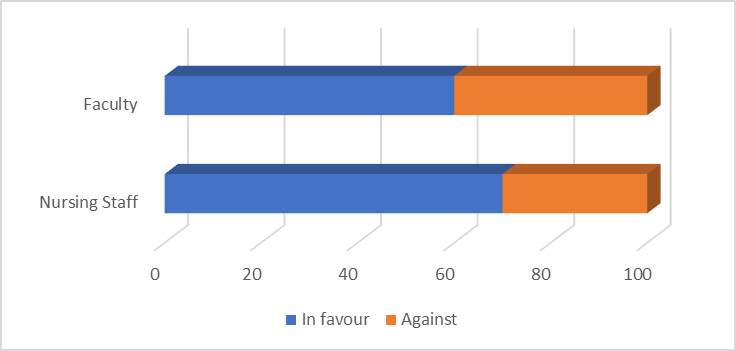
Figure 2: Opinion poll of faculty and nursing staff for peer tutoring.
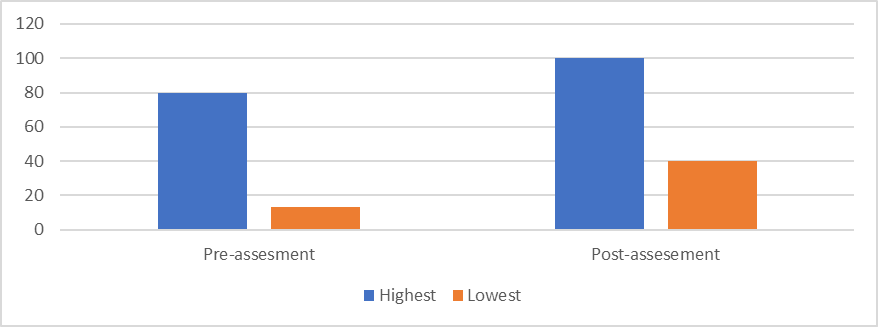
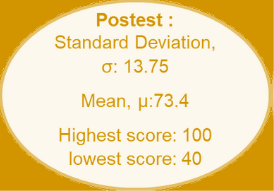
Pre-Test and Post-Test Scores: Pre-test and post-test assessments demonstrated significant learning outcomes. Pre-test scores ranged from 13 to 80, with a mean of 56.05 (SD = 16.08). In contrast, post-test scores ranged from 40 to 100, with a mean of 73.4 (SD = 13.75), illustrating substantial improvement (Figure 3).
Figure 3: Assessment of Pre and Post Test questionnaire for analyzing the impact on tutees

Tutor Self-Assessment: Tutors self-assessed their performance, aligning largely with tutee feedback regarding strengths in communication and subject command. However, tutors acknowledged the need for improvement in time management and teaching aid utilization, corroborating HICC and MEU observations.
DISCUSSION
Peer tutoring (PT) has gained recognition as an effective educational modality in various settings, particularly in resource-limited environments where faculty resources are stretched. In the context of infection prevention and control and control (IPC) training, our study provides compelling evidence that peer tutoring can enhance healthcare professionals’ adherence to IPC practices. This aligns with previous research demonstrating PT’s effectiveness in promoting knowledge and behavioural changes among healthcare staff, particularly in domains such as hand hygiene, biomedical waste management, and safe injection practices.1
One of the key findings of this study was the significant improvement in post-test scores among tutees, indicating that the peer tutoring model successfully transferred knowledge. This result mirrors findings from Shenoy et al., who reported similar gains in knowledge among medical students involved in peer-assisted learning (PAL) programs.3 The ability of peer tutors to communicate complex topics in a relatable way, due to their cognitive congruence with their peers, likely contributed to this success. Cognitive congruence refers to the peer tutor’s capacity to explain concepts using language and examples that resonate with tutees, a feature often absent in traditional faculty-led training.4 This shared understanding fosters a learning environment that encourages greater engagement and retention of knowledge.5
High satisfaction levels among tutees, as evidenced by their ratings on the Likert scale, further underscore the effectiveness of peer tutoring in this context. Participants appreciated tutors’ command of the subject matter and their ability to link theoretical knowledge with real-life experiences. This finding is consistent with Breckwoldt et al.’s study, which found that peer tutors who could relate IPC training to practical examples had better success in engaging their peers.6 However, the study also identified areas for improvement, particularly in time management and the utilization of teaching aids. Similar challenges were reported by Glynn et al., who found that peer tutors in their program struggled with time allocation, often rushing through important content to stay on schedule.7
Despite these challenges, the peer tutoring model was widely accepted by both tutors and tutees. This acceptance is critical in environments with limited faculty resources, as it offers a sustainable alternative to traditional teaching methods. Furthermore, peer tutoring promotes a sense of ownership and accountability among healthcare staff, as evidenced by opinion polls conducted in our study. This sense of ownership is essential for long-term adherence to infection prevention and control practices, as it encourages healthcare professionals to take personal responsibility for preventing hospital-acquired infections (HAIs).8 This finding aligns with other research suggesting that peer-led programs promote behavioural change through social congruence, where peer tutors and tutees share similar social backgrounds and professional responsibilities.9
Interestingly, our study found that nursing staff were more receptive to peer tutoring than doctors. This disparity in attitudes may stem from nurses being more directly involved in IPC practices on a day-to-day basis. Glynn et al. also reported that nurses tend to be more engaged in peer-assisted learning programs, particularly when focusing on practical skills like IPC.7 However, this finding raises important questions about how to better integrate doctors into such programs, given their crucial role in IPC compliance.10
The broader implications of our study suggest that peer tutoring in IPC can lead to significant long-term impacts, including reduced rates of HAIs, decreased patient length of stay, and a lower financial burden on both patients and healthcare institutions. These benefits are consistent with the literature on peer-assisted learning, which has shown that peer-led educational programs can lead to lasting improvements in clinical practice.4, 11 Moreover, the potential for peer tutoring to reduce antimicrobial resistance by promoting adherence to infection prevention and control protocols is particularly relevant in low-resource settings where HAIs and antimicrobial resistance are major public health concerns.12
However, our study has limitations. First, the peer tutoring program was implemented over a relatively short period of six months, which may not capture the long-term effects of peer tutoring on infection prevention and control behaviour. Additionally, while we focused on the nursing staff, future studies should consider expanding the scope to include other healthcare professionals, such as doctors and ancillary staff, to obtain a more comprehensive view of the program’s impact. Finally, reliance on self-reported data, such as satisfaction surveys and self-assessments, introduces the possibility of bias, as participants may overestimate their performance or satisfaction due to social desirability.13
CONCLUSIONS
Our study highlights the potential of peer tutoring as a method for improving infection prevention and control practices in low-resource hospital settings. By leveraging the expertise of motivated healthcare professionals as peer tutors, institutions can address challenges posed by faculty shortages while still providing high-quality training to their staff. Future research should explore the scalability of this model and its long-term impact on infection rates and antimicrobial resistance.
ACKNOWLEDGEMENT
Nursing Officers Mr. Soyab Khan, Ms. Nisar Jahan, Mr. Anwar, Mr. Pradeep Kumar for their support. The study was presented at the Advance Course in Medical Education (ACME) Workshop at NHLMMC, Ahmedabad, 26th to 27th July 2024. We also acknowledge Prof. Neeraj Mahajan, NHLMMC, Ahmedabad, for mentoring the project.
CONFLICTS OF INTEREST STATEMENT
The authors declare no conflict of interest.
SOURCE OF FUNDING
None
AUTHOR’S CONTRIBUTION
FK: Study planning, implementing, data analysis , writing
A: Writing the manuscript and assessing in video analysis
SA : Data analysis and Review
MSS:: Study Planning, Data Analysis, Review
TK: Study Planning, Review
REFERENCES
Centers for Disease Control and Prevention. Occupational infection prevention and control: Education and training [Internet]. 2024 [cited 2024 Aug 17]. Available from: https://www.cdc.gov/infection-control/hcp/healthcare-personnel-infrastructure-routine-practices/occupational-training.html
Joseph HA, Shrestha-Kuwahara R, Lowry D, Lambert LA, Panlilio AL, Raucher BG, et al. Factors influencing health care workers’ adherence to work site tuberculosis screening and treatment policies. Am J Infect Control. 2004 Dec;32(8):456-61. doi: 10.1016/j.ajic.2004.06.004.
Shenoy A, Petersen KH. Peer Tutoring in Preclinical Medical Education: A Review of the Literature. Med Sci Educ. 2019 Dec 23;30(1):537-44. doi: 10.1007/s40670-019-00895-y.
Loda T, Erschens R, Loenneker H, Keifenheim KE, Nikendei C, Junne F, et al. Cognitive and social congruence in peer-assisted learning – A scoping review. PLoS One. 2019 Sep;14(9):e0222224. doi: 10.1371/journal.pone.0222224.
Nathavitharana RR, Bond P, Dramowski A, Kotze K, Lederer P, Oxley I, et al. Agents of change: The role of healthcare workers in the prevention of nosocomial and occupational tuberculosis. Presse Med. 2017 Mar;46(2 Pt 2):e53-e62. doi: 10.1016/j.lpm.2017.01.014.
Breckwoldt J, Knecht M, Massée R, Flach B, Hofmann-Huber C, Kaap-Fröhlich S, et al. Operating room technician trainees teach medical students – an inter-professional peer teaching approach for infection prevention strategies in the operation room. Antimicrob Resist Infect Control. 2019 May 14;8:75. doi: 10.1186/s13756-019-0526-2.
Glynn LG, MacFarlane A, Kelly M, Cantillon P, Murphy AW. Helping each other to learn – a process evaluation of peer assisted learning. BMC Med Educ. 2006 Mar 10;6:18. doi: 10.1186/1472-6920-6-18.
Aljahany M, Malaekah H, Alzahrani H, Alhamadah F, Dator WL. Simulation-Based Peer-Assisted Learning: Perceptions of Health Science Students. Adv Med Educ Pract. 2021 Jun 30;12:731-7. doi: 10.2147/AMEP.S308521.
Herrmann-Werner A, Gramer R, Erschens R, Nikendei C, Wosnik A, Griewatz J, et al. Peer-assisted learning (PAL) in undergraduate medical education: An overview. Z Evid Fortbild Qual Gesundhwes. 2017 Apr;121:74-81. doi: 10.1016/j.zefq.2017.01.001.
Breckwoldt J, Gruber H, Wittmann A. Simulation learning. In: Billett S, Harteis C, Gruber H, editors. International Handbook of Research in Professional and Practice-based Learning. Heidelberg: Springer; 2014. p. 673-98. doi: 10.1007/978-94-017-8902-8_25.
Avonts M, Bombeke K, Michels NR, Remmen R. How can peer teaching influence the development of medical students? A descriptive, longitudinal interview study. BMC Med Educ. 2023 Dec 21;23:861. doi: 10.1186/s12909-023-04801-4.
Alhumaid S, Al Mutair A, Al Alawi Z, Alsuliman M, Ahmed GY, Rabaan AA, et al. Knowledge of infection prevention and control among healthcare workers and factors influencing compliance: a systematic review. Antimicrob Resist Infect Control. 2021 Jun 3;10(1):86. doi: 10.1186/s13756-021-00957-0.
Ahmed OM, Juthani PV, Green ML, Moeller JJ. Optimizing preclinical learning with retrieval practice: A call to action. Med Teach. 2021 Jun;43(6):718-20. doi: 10.1080/0142159X.2020.1788212.
Submit a Manuscript:
Copyright © Author(s) 2025. JASPI- Journal of Antimicrobial Stewardship Practices and Infectious Diseases.

